|
There are many abbreviations used to describe vaginal births after a cesarean. Here are some to know before reading this article: VBAC - Vaginal birth after cesarean VBAC-2 - Vaginal birth after two cesareans TOL - Trial of labor When it comes to deciding where and how someone welcomes their baby into the world, there are many factors to consider. Birthing parents deserve to know their options and what the risks and benefits of each option are, but it can be hard to figure out where to start when researching providers and asking questions. When it comes to discussing a VBAC there are a lot of questions someone may be thinking about. Here are our top 8 questions to ask your provider, and why you should ask them. Is your provider VBAC supportive? Your provider may not feel comfortable supporting a VBAC, but that does not mean it is not an option for you. You may want to consult with multiple providers. We also recommend making sure other providers in the practice are supportive because the provider attending your birth might be whoever is on call. Is your provider VBAC supportive after more than one c-section? Some providers may feel comfortable attending a VBAC after one cesarean, but that support can change after two cesareans. Have they attended a VBAC before? How many were successful? How many were successful in the past year? It is important to make sure you are confident in your provider's skill set and that they have a proven track record that would allow you to have your desired outcome for your birth. Always remember, you have options when it comes to birth and who attends your birth. If your current provider's views do not align with your own, but you meet the qualifications for a cesarean set by the American College of Obstetricians and Gynecologists, you may want to look into other providers in your area. You can also reach out to ICAN, the International Cesarean Awareness Network. They have local chapters and they may provide you with a list of local VBAC supportive providers. You can also join their Facebook group to receive support from other VBAC families. What are the risks? What are the benefits? Research is constantly being released. Make sure that you are up to date on what the benefits and risks for a VBAC are, and what risks are specific to you. A provider who knows your history is the best person to answer this question. Gentle Cesareans involve skin to skin in the OR, a clear curtain, and sometimes delayed cord clamping. This may be worth asking about beforehand to prepare in the event that a repeat cesarean does occur. How far past your due date will they recommend you go before a repeat cesarean is recommended? If you go past your due date would they recommend trying an induction first? This question allows you to better know what to expect and ask questions accordingly. If you have the option to be induced you may wish to request that before you reach your due date or you may have questions about what to expect if an induction does occur (if you have not had one before). If being induced is an option there are different routes, one may be an option for you while others may not be. It is important to know what those are. If induction is a no altogether, you may want to know that sooner rather than later. What type of monitoring do you recommend for VBAC patients? Knowing what monitoring is recommended, and will most likely be used, allows you to plan accordingly for different labor positions. If you are going to be restricted to a bed it may be important to you to research bed labor positions, peanut balls, etc. How long are they comfortable letting patients labor for, after their water breaks? This is another question you may want to ask to prepare yourself for what to expect. This may also determine your decision to use Pitocin or request an epidural. Pitocin is typically used to “speed up” labor. An epidural is used for pain management, but can slow down contractions. Someone might not want an epidural if they have a small time limit after their water breaks. What policies should you be aware of that may make a VBAC harder to achieve? Or, what policies should you be aware of? The hospital or birthing center you are delivering at may have policies that make a VBAC harder to achieve. There may be policies preventing movement or hydrotherapy. The policies may make you more likely to request an epidural. This may impact someone's decision to give birth there or impact the preparation they do to plan pain management techniques. For any birthing parent, it is important to know when providers recommend you arrive, based on your medical history. You may also want to know about policies around eating in labor. Around 70% of birthing parents who elect for a trial of labor are successful. Research is constantly being published showing that a VBAC is safe if the birthing person meets a set of qualifications, these qualifications may differ depending on the practice you attend and a provider's comfort level. You may be a good candidate if:
Risks may include:
The Mayo-Clinic has listed the following benefits:
References:
ACOG, Midwifery Today, Winter No 36, page 47. Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol 2001;97(3):439-42. Habak PJ, Kole M. Vaginal Birth After Cesarean Delivery. [Updated 2021 Aug 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507844/ International Cesarean Awareness Network , I. C. A. N. (2021, March 19). Advocacy. International Cesarean Awareness Network. Retrieved January 31, 2022, from https://www.ican-online.org/advocacy/ Mayo Clinic (2020, June 9). Vaginal birth after cesarean (VBAC). Mayo Clinic. Retrieved January 31, 2022, from https://www.mayoclinic.org/tests-procedures/vbac/about/pac-20395249 Stamilio DM, Shanks A. Vaginal birth after cesarean (VBAC) outcomes associated with increasing number of prior VBACs. Womens Health (Lond). 2008 May;4(3):233-6. doi: 10.2217/17455057.4.3.233. PMID: 19072472.
0 Comments
What to Know About Poor Egg Quality2/4/2023 Poor egg quality can make or break if a pregnancy can make it to term. It is typically caused by low ovarian reserve. Every menstruating human has some abnormal eggs. At age 20 about 20% of eggs are considered abnormal, but by 40 that number has risen to 80%. By age 35 only 6% of a person's total eggs remain! Knowing about poor egg quality may be important if you are struggling to conceive and want to know what to expect or what to ask your doctor about. It may also be important if you are deciding to have children now or later. There are many reasons why it may be important to improve your egg quality. It may be vital for you to improve egg quality if you are over 35, you have a diminished ovarian reserve, you have low AMH (anti mullerian hormone), your cycle is getting shorter, or you have had a failed round of IVF. Egg quality drives fertility. Eggs with abnormal DNA (aneuploidy) are not likely to even fertilize. There is no clear consensus on average egg count for those with diminished ovarian reserve. What are the signs of poor egg quality?
Poor egg quality causes a fertilized egg to either not implant or only partially implant. If it does implant it usually will not develop properly. This typically leads to miscarriages or birth defects. Research has shown the rates of biochemical pregnancy, clinical pregnancy, and embryo implantation in young people with DOR are significantly higher than in older people with DOR. Young people with DOR have ovarian hypo-response and low numbers of acquired eggs and embryos, but the possibilities of high-quality embryo and good clinical pregnancy are higher once eggs are acquired, according to research published in 2018. Biochemical pregnancy is where the egg implants, but is miscarried in the first 2-3 weeks after conception. Clinical pregnancy is a pregnancy confirmed by HCG (Human Chorionic Gonadotropin) levels. Embryo implantation is described as an embryo implanting in the uterus. Embryo is used to describe a developing fetus before the eighth week, when we typically describe it as a fetus. Low Ovarian Reserve Low ovarian reserve or diminished ovarian reserve (DOR) is used to refer to the number of eggs someone has. About 10% of people with ovaries experience this, according to the Center for Human Reproduction. Treatments do not exist, but recommendations to live a healthier lifestyle can be made. Those recommendations boost fertility and improve conditions for the egg that will be released in ovulation. It is important to improve these conditions three months before ovulation. Causes of Low Ovarian Reserve Include:
Poor egg quality can lead to chromosomally abnormal pregnancies. It can also increase the risk of genetic disorder in the baby. Most chromosomal errors occur three months before ovulation when either a chromosome doesn't separate and pair up again properly in meiosis, or chromosomes break, become inverted, or get deleted due to chemicals and viruses. Changing the conditions of the egg three months before ovulation can improve that egg's quality and decrease the chance of chromosomal abnormality. Mitochondria is responsible for the energy used to produce a good quality egg. If mitochondria is damaged, egg quality is poor. Nutrition and lifestyle factors play a role in egg quality. IVF IVF, or in vitro fertilization, allows the best egg to be hand picked. Meaning, while those with poor egg quality may not have as many good embryos they can still get pregnant through IVF. InGenes says, “Patients with poor egg quality have a higher rate of structural genetic abnormalities; however, by transferring chromosomally normal embryos, this technique maximizes the chance of embryo implantation..." Testing A blood test to measure a patient's follicle stimulating hormone (FSH) and estradiol blood levels are performed on day 3 of their cycle to determine ovarian response and egg quality. You can also take an at home ovarian reserve test. Other forms of testing may include, AMH (anti mullerian hormone) blood level testing and antral follicle count, an ultrasound that looks at the number of visible antral follicles to predict primordial follicles (microscopic follicles that each contain an immature egg). How can you improve egg quality and maximize fertility:
New Research and Fertility Medications for Better Egg Quality The Center for Reproductive Health believes early diagnosis is important for those with diminished ovarian reserve (DOR). 33% of their patients with DOR have successful pregnancies with their own eggs. Dehydroepiandrosterone (DHEA), a mild androgen as proven success for those with DOR. A 2010 study showed that 23.1% of the participants who took DHEA supplements had a live birth, those who didn’t take DHEA had a 4% live birth rate. In 2012 a review concluded that more research on DHEA is needed. Coenzyme Q10 (CoQ10) is an antioxidant powerhouse that can increase egg quality. In a human trial, supplementation with CoQ10 led to higher fertilization rate and more high-quality embryos. CoQ10 also has increased the number of ovarian follicles and improved ovulation. Research, published in the journal Nature, has found boosting levels of a common metabolic coenzyme may help improve egg quality and chances of conception naturally and through IVF. Researchers from the University of Queensland’s Center for Clinical Research found that the quality of a woman’s eggs is significantly dependent on nicotinamide adenine dinucleotide (NAD+). NAD+ is a chemical found in every cell of the body. NAD+ is involved in hundreds of metabolic processes and declines with age. Research showed that boosting NAD+ in mice returned their eggs from 40 year old quality to 30 year old quality. Using donor eggs is another option for those with poor egg quality. Choice of treatment is specific to each person, their medical history, and their fertility goals. It is always best to consult with your provider about your options. If you feel that your provider is not best for you, you can always consult with more providers until you find the best fit. Can you preserve egg quality? Cryopreservation is a technique to preserve egg quality. It is the process of freezing your eggs. Frozen eggs do not lose their quality with age and can be used later when your fertility and egg quality have declined. Understanding your egg quality is an important step in trying to conceive and determining when you plan to try to conceive. Someone with low ovarian reserve may choose to freeze their eggs if they want to have children later, in order to preserve their quality. Someone else may choose to have children earlier. Decisions around fertility are personal and require a lot of thought. A confident decision is made when someone has all of the information and has asked all the questions they need to. Here are some questions you may want to ask your provider as a start:
References:
Bolton, R. (2021, October 19). The facts about egg quality. Plan Yourself Pregnant. Retrieved February 2, 2022, from https://www.planyourselfpregnant.com/the-facts-about-egg-quality/ Camargo, F. (2020, March 26). Poor quality eggs causes and treatment to conceive a baby. Ingenes. Retrieved February 3, 2022, from https://www.ingenes.com/international/are-you-a-candidate/female-infertility-causes/poor-egg-quality/ Chang, Y., Li, J., Li, X., Liu, H., & Liang, X. (2018). Egg Quality and Pregnancy Outcome in Young Infertile Women with Diminished Ovarian Reserve. Medical science monitor : international medical journal of experimental and clinical research, 24, 7279–7284. https://doi.org/10.12659/MSM.910410 CNY Fertility (2022, January 28). How to improve egg quality after 40. CNY Fertility. Retrieved February 3, 2022, from https://www.cnyfertility.com/how-to-improve-egg-quality-after-40/ Contributor, S. C. R. C. (2017, July 25). How to improve egg quality for pregnancy or IVF. How to Improve Egg Quality for Pregnancy or IVF. Retrieved February 3, 2022, from https://blog.scrcivf.com/how-to-improve-egg-quality-pregnancy-ivf Ferguson, S. (2019, February 26). Diminished ovarian reserve: Overview, causes, and treatments. Healthline. Retrieved February 3, 2022, from https://www.healthline.com/health/diminished-ovarian-reserve#treatment Rasool, S., Shah, D. Fertility with early reduction of ovarian reserve: the last straw that breaks the Camel’s back. Fertil Res and Pract 3, 15 (2017). https://doi.org/10.1186/s40738-017-0041-1 Tsirtsakis, A. (n.d.). Metabolic coenzyme shows promise for improved egg quality. NewsGP. Retrieved February 3, 2022, from https://www1.racgp.org.au/newsgp/clinical/metabolic-coenzyme-shows-promise-for-improved-egg The Role of AMH in Fertility2/4/2023 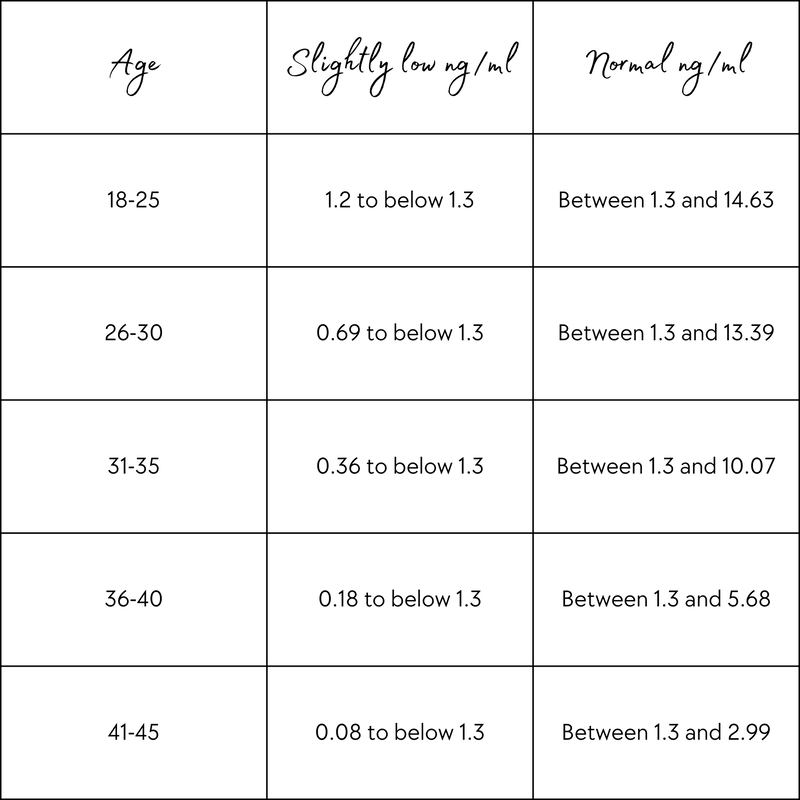 If you’re looking into information about trying to conceive and your fertility, you may have come across the letters A-M-H. Those letters stand for anti mullerian hormone, a hot topic in the medical community right now. Research is showing that AMH levels can help determine ovarian reserve quality, but there is a push for more research to be done. Knowing your anti-mullerian hormone levels can be an important step in your fertility journey. It can allow your provider some insight into what may be preventing you from conceiving, allowing a plan to be created to help you along your fertility journey. Let’s take a look at what exactly AMH is and why it may be important for you to look into. What is AMH? AMH stands for anti mullerian hormone. AMH plays a very important role in the regulation of ovarian follicle growth. AMH levels can help a doctor determine egg count. According to Advanced Fertility, “AMH blood levels are thought to reflect the size of the remaining egg supply – or “ovarian reserve””. It used to be referred to as “mullerian inhibiting substance” or “MIS”. What is a typical AMH? The typical AMH in a fertile person is 1.0-4.0 ng/ml. Dr. Nataki Douglas of Modern Fertility recommends testing once, then again in about 12 months. When you should consider retesting depends on your age, your AMH level, and how it is changing over time. Why would you test your AMH? AMH testing can be used to determine the start of menopause, determine reasons for early menopause, find out the reason for lack of menstruation (amenorrhea), diagnose poly-cystic ovarian syndrome (PCOS), check infants with genitals that can not be determined as male or female at birth, and to monitor ovarian cancer. It is often used to diagnose amenorrhea in females younger than 15 and to diagnose PCOS in those trying to conceive. You may want to request an AMH test if you are experiencing decreased breast size, weight gain, facial and body hair growth, acne, and menstrual disorders or irregular periods. You may also need testing before beginning IVF (in vitro fertilization). It is important to know that AMH levels can fluctuate. Your levels right now are not an end all on if you are able to conceive. That is why it is important to track AMH. Fertility begins to decline up to 10 years before menopause and the average age of menopause is 51. By 41 fertility is already taking a major decline. With so many people waiting longer to start a family, AMH is becoming more important to monitor in order to be successful in your pregnancy journey. It may determine if someone chooses to start a family earlier rather than later. What to know about low AMH
What to know about high AMH
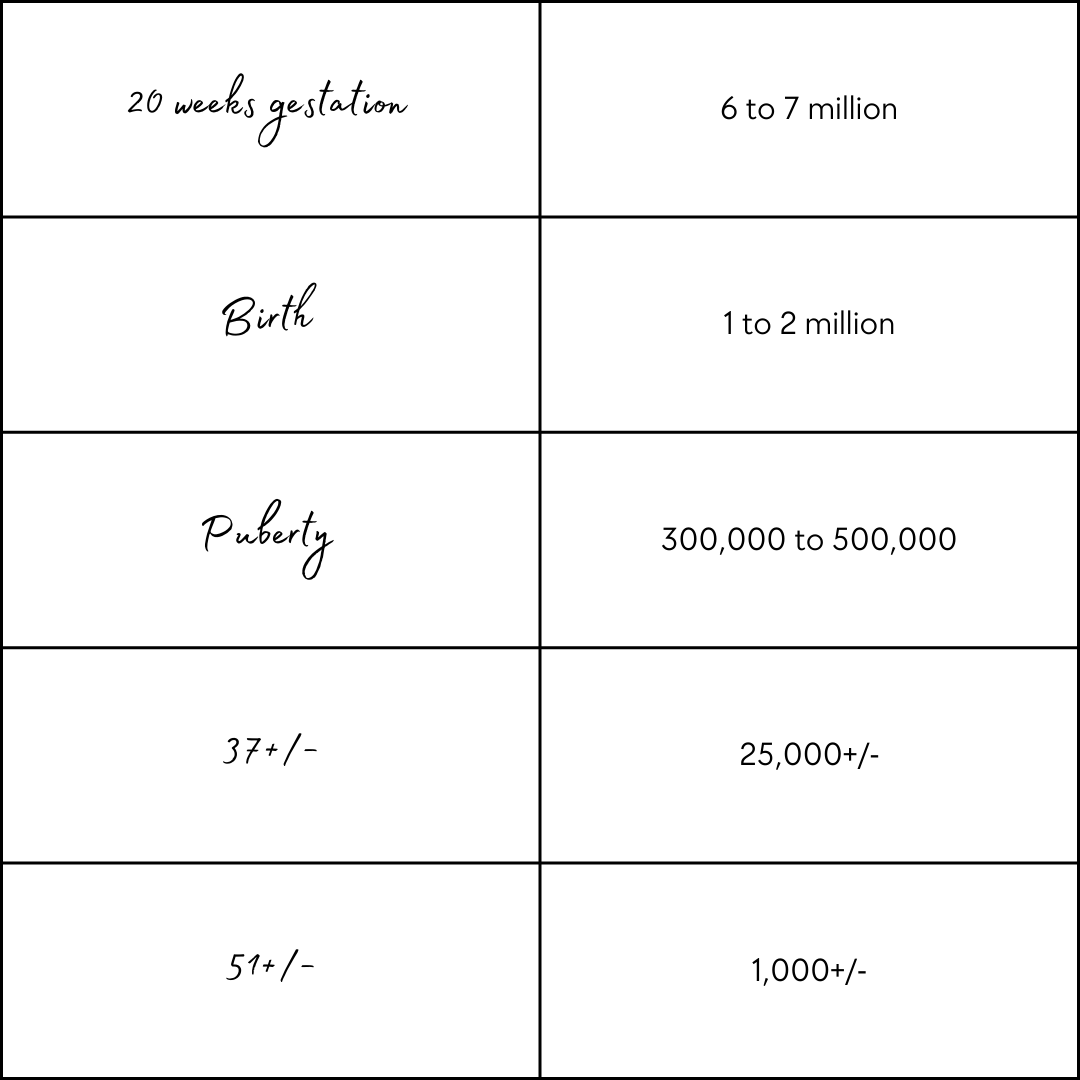
Increasing AMH Some research has shown taking micronutrients present in Impryl can increase AMH. Poor nutrient absorption can contribute to low AMH, as seen in people with Crohn’s disease. It is important to consult with specialists if you have an autoimmune disease because treating your autoimmune disease, if possible, may improve your AMH levels. The Journal of Human Reproductive Sciences published a study showing increased AMH when people began exercising moderately. There is no conclusive evidence of if AMH levels can be increased, but proper diet and exercise can prepare your body for a healthier pregnancy. IVF and AMH AMH can help you understand how many eggs may be extracted during egg retrieval for egg freezing and IVF. Your AMH levels may be checked during your initial lab work when pursuing IVF. These levels can determine if you are a good IVF candidate. In IVF patients high AMH levels correlate with low cancellation rates, retrieval of more eggs, higher live birth rates and a high chance for freezing of leftover embryos. Research shows no difference in success for patients with low vs extremely low AMH. Age is a key factor in the success of IVF. Past Pregnancy Delivery Mode There has not been a connection found thus far between type of delivery and AMH levels. A past cesarean section would not impact levels over a vaginal delivery. Birth Control and AMH The oral birth control pill has been shown to lower AMH levels temporarily. This differs brand to brand and person to person. It is important to consult with your doctor when making decisions about which birth control option is best for you and for your future fertility goals. Testing Methods Testing is usually conducted via a standard blood sample. Testing can be conducted at home with kits like the Modern Fertility Hormone Test. Egg Count
Throughout trying to conceive there are so many questions people want to ask and they want detailed answers. People do not want a “we just don’t know” type of answer from their provider, which is why further research is so important. People deserve to know what is going on in their body. It can be hard to know what to ask when consulting with a provider and in lots of cases, if you don’t ask they might not tell you something you wish you had known. Anti mullerian hormone is a key term to know when trying to conceive, especially for those of us experiencing infertility. Remember that you can always ask your provider if AMH testing is right for you, order an at home test, or consult with other providers if you think AMH testing could bring you a clearer picture of what is happening inside your body. 7 Tips for Strengthening Your Relationship with Your Partner: Starting In The Postpartum Period2/4/2023 The postpartum period is a huge transition and it can feel hard to find the time to focus on all of the things you want to. You want to focus on healing yourself mentally and physically, bonding with your baby and unfortunately, something that often gets neglected is your relationship with your partner. Now, I do believe that having a steady foundation is key and that when that foundation is in place you should not be worried about it crumbling, but we all want to feel loved and know that we are seen. When it comes to expressing love and showing someone that we truly appreciate them we do not need to hire someone to serenade them or buy a million roses. There are simple things we can incorporate into our daily routine that will make our partner feel seen. I cannot stress enough that you cannot pour from an empty cup. As a society, we constantly expect parents to do this. One parent puts in a huge effort without asking the other for help and feels completely drained, then the other parent picks up a little of the load to pull the drained parent back up but that drains this parent and then they are trapped in a vicious cycle of being drained, then filled, then drained again. It is important to find some balance. Incorporate healthy sustainable methods of caring for one another throughout pregnancy so that those methods are part of your daily routine and do not feel like an added stressor or a chore on your to-do list. But what even are healthy ways to strengthen your relationship without emptying your cup. 1. Over Communicate! Before the baby arrives, after the baby arrives - just constantly communicate! Set the expectations of what you want your partner to do postpartum. Is it usually expected that you handle laundry? Let your partner know that you will be passing that task on to them. Keep the communication going postpartum. It is important to have a safe space to communicate in. With so much going on there are times that just are not ideal for having big talks, like when your baby has a blowout and is inconsolable. Set boundaries and create times and spaces that you have laid out with your partner so you both know when to have those bigger talks. Communication even extends to text. Text each other messages of gratitude. This helps strengthen your connection when a partner is not home. Remember, your partner cannot read your mind. Just because you are thinking about how thankful you are, does not mean they know that. Tell them how you are feeling! 2. Educate Yourself! This is what you are doing by reading this post right now. You are preparing and researching. There are going to be issues that arise postpartum that are different from issues you and your partner have had in the past. Educate yourself on what to expect so that you can fill your toolkit with healthy coping techniques if/when those issues arise! 3. Take Time For Yourself! The theme stressed here has been not pouring from an empty cup. Self-care is an important way to fill your cup. Allow your partner time one on one with the baby so that you can go do something by yourself. This could be getting lunch with a friend, going for a walk, taking a nice bath, napping, or catching up on a book or show you like. 4. Prioritize Dates With Your Partner! It can be hard to find time to go out on a date, but you don’t always need to leave the house to have a date night. If you aren't comfortable having a sitter come you can try having more of a mother's helper or have a family member come. Have them watch the baby while you and your partner enjoy dinner together, a nice shower, or even just a nap. Back in my babysitting days, I had a few families I worked with that would have me watch their newborn while they enjoyed a picnic outside together or put a movie on downstairs while I watched the baby up in the nursery. I even had one family camp in the backyard while I watched their twins overnight inside! Get creative and have fun with it! Some of my favorite date nights have been ones where my partner and I learned a new recipe at home together or nights where we make smores together in the living room fireplace! Coming up with creative ideas shows your partner how thoughtful you are and how important this is to you. 5. Do Things As A Family! It can feel easy to get stuck in a pattern of one parent being with the baby at a time, especially when one parent is working. Plan activities to do together. This will lighten your load by giving you an extra set of hands during outings, but this also makes your partner feel included. After carrying your baby for nine months and birthing them your partner is probably excited to be even more involved now that the baby has arrived. These moments allow you to all feel connected, as a whole family which furthers the bond between you and your partner. You should feel like a united front in this new territory. 6. Set Realistic Ways For Your Partner To Help! If you are doing the nighttime feeds, have your partner get up with the baby in the morning. This is a realistic, healthy way to manage your baby’s needs, support each other, and help each other get adequate sleep. Social media can create unrealistic expectations of what a partner should do. Talk to each other about what is realistic to ask of each other. Remember, unless you set specific tasks to each do, you are a team and should both be responsible for tasks. 7. Prioritize Intimacy! Intimacy is not just physical, but also emotional. When it is safe to do so, have sex if you want to. Take this as an exciting time to explore what is comfortable and what you enjoy, it may be something different than what you have enjoyed in the past. This is another time when communication is extremely important. Remember that sensations may be different as things have changed during pregnancy and birth. If you are concerned, consult with your provider. Communication is a way many people connect emotionally, but that may not work for you. Explore your Love Language. It could be physical touch, words of affirmation, acts of service, quality time, or gifts. Talk to your partner about how they can best show you love and ask them how you can do the same. You may be trying hard, but not using their love language. Another great way to connect emotionally is to stay curious about your partner. Ask questions and show interest in what they are doing. Ask them how they are doing and listen to their answer. Postpartum is a hectic time full of wild changes, but it is a time that deserves to be remembered and enjoyed. One of the steps to enjoying this period is connecting with your partner and strengthening the team you both are part of. So many people end up blocking out the postpartum period because it was stressful and too much at times, but it is one of the most transformative moments of your life. We make a huge effort to remember our wedding day, prom, and graduation because they are big moments, yet we block out postpartum. Why is that?
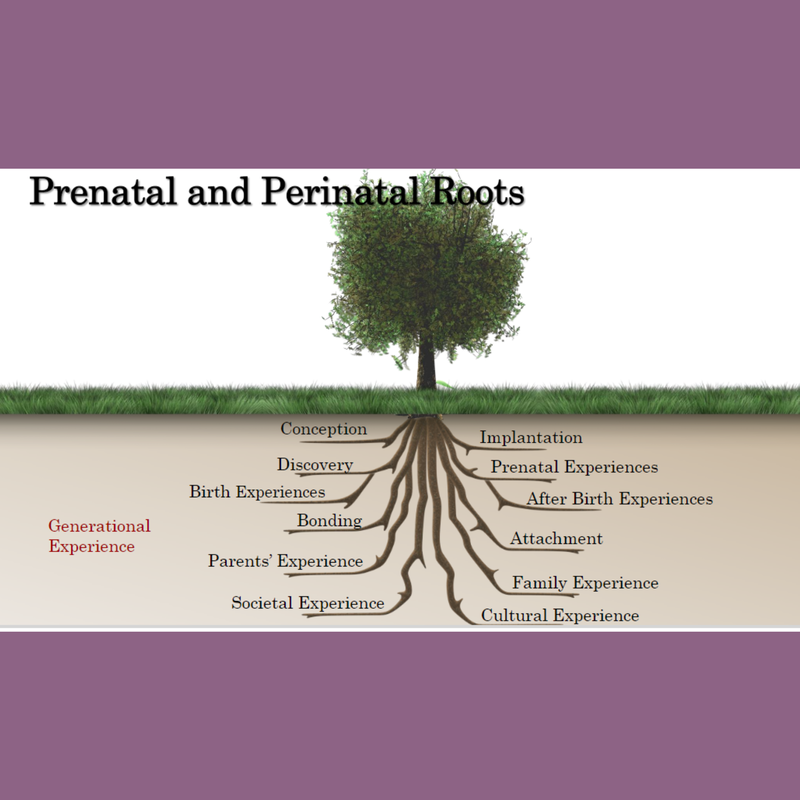
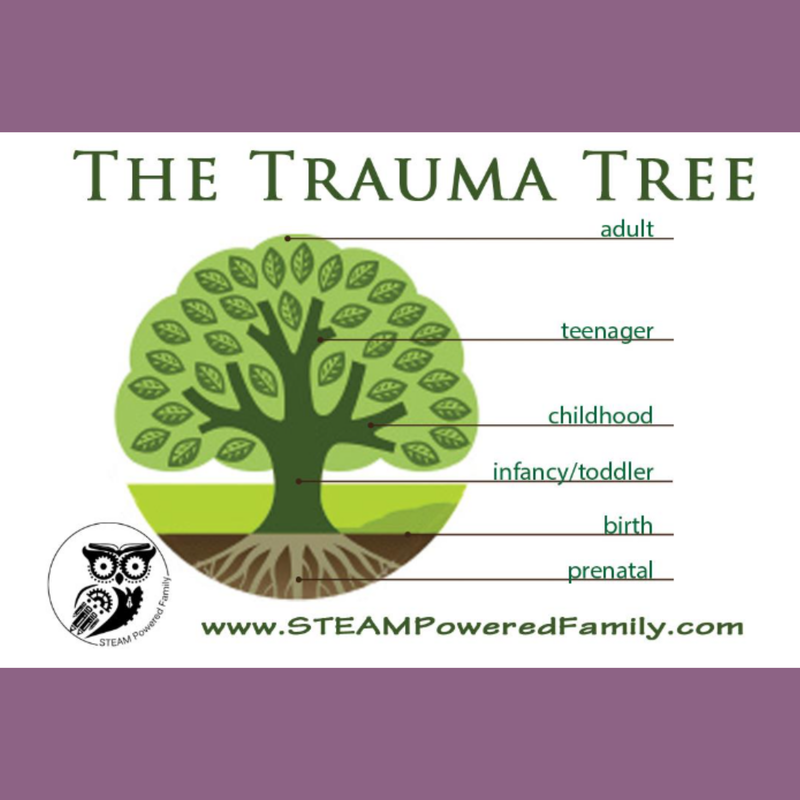
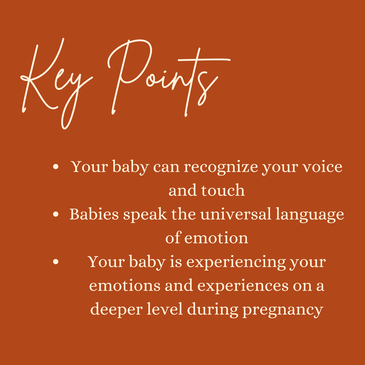
Let’s make an effort to better prepare parents and provide them with resources to ease this transition for the whole family, starting with the foundation of the family; the parents. Bonded Birth - A toolkit2/4/2023 The infant-to-parent bond is one of the strongest bonds we see in life. It helps shape emotional regulation, sleep, mental health, and even more for both parents and babies. Often times we see parenting courses skim over this very important part of parenting. In this resource we will cover: - How we know babies are conscious - Exercises for exploring consciousness with your baby - Bonding through pregnancy - Bonding through labor and birth - Bonding throughout the first year postpartum - Bonding for non-gestational parents The DNA selection for an embryo is impacted up to three months prior to conception. Healing our trauma prior to conception is a great step to ending generational trauma. The DNA selection for an embryo is impacted up to three months before conception. Imagine how greatly it is also impacted in pregnancy!Developmental Milestones and Opportunities for Connection:Tactile sensitivity begins in the seventh week of gestation and steadily enlarges to include most parts of the body by seventeen weeks and all parts by thirty-two weeks. There are many ways to see a physical reaction and know for yourself that your baby is responding. Talk to your baby! Hearing may begin early in the first trimester or as late as eighteen weeks. Speaking to your baby is a great way to begin bonding. Your baby will begin recognizing your voice specifically. This is a great way to check in with your baby about the emotions you are experiencing. Stress is a normal part of life, but telling your baby what is happening and why can reduce the impacts of stress long term. Interact with your baby! The fetus is aware of light even while the eyelids are still fused and will react to lights flashed on the abdomen. You can try playing with a flashlight on your abdomen, moving your hands along your abdomen and following baby as they follow the light. You can also try interacting through noise such as music. You may find your baby prefers Taylor Swift over Beethoven or vice versa! Dreaming Premature babies dream more than anybody else! They show the most smiles, frowns, finger movements, neck stretches, mouth movements, and vocalizations in their dreams. Ultrasound has shown that the beginning of REM/dreaming activity is at just twenty-three weeks! Medical Interventions Babies in the womb react to medical interventions with accelerated heart activity, turning, or moving away. This can be seen when a fetus moves away from the ultrasound probe or bats it away. Many parents who notice this will opt out of ultrasound and testing that could be disruptive to their baby, but others may choose to talk to the baby throughout the procedure; to let them know what is happening and why. Your baby is connected with you and is experiencing your emotions on an even deeper level. While it can be important and effective to reduce stress and keep a positive mindset it can also be important to discuss feelings and experiences directly with your baby. This not only teaches emotional regulation, but also offers more bonding opportunities.
Karen Strange's 4 Ways to Communicate with Baby 1. Tell your baby what you are going to do BEFORE you do it 2. Tell your baby what is going on 3. Tell your baby what you want them to do 4. Tell your baby the story of what happened Reduce mother and baby separation. The first hour postpartum is when skin to skin is the most important, and especially throughout the first 24 hours. Many policies and procedures are in place for hospital financial gain and efficiency. You have consent and you can say no to something. You can also request that routine procedures be done on you! If baby needs to be measured, temperature checked, etc those tasks can be done with baby on your abdomen with minor adjustments from staff. Bonded Birth Goals:
Birth Plan Considerations for a Bonded Birth:Remember, the best birthing experience is one where you are making choices that are right for you and your family. Pain medication and the breast crawl are two important parts of a birthing plan that may not be thought about when it comes to birth psychology. They should be considered! 1. Pain Meds: Pitocin, the synthetic form of Oxytocin commonly used to induce labor, uses all the oxytocin receptor sites. Oxytocin breaks the blood/brain barrier and offers relief, but Pitocin does not. Oxytocin is commonly referred to as the love or cuddle hormone. It is released in the highest doses during orgasm, childbirth, and breastfeeding. It is essential for bonding and should remain flowing through labor and immediately postpartum. It can reduce risk of PMADs (perinatal mood and anxiety disorders) and prevent hemorrhaging. The endorphins naturally released throughout labor reduce pain in birthing parent and in baby, and encourage bonding! Pain medication may prevent baby or birthing parent from being an active member in the birth, prevent endorphin release, delay milk/lactogenesis, relaxed pelvic floor making it harder for baby to rotate, impact on heartrate, and impact on head molding which impacts ability to suck and swallow. 2. Breast Crawl: Breast crawl is the instinctive movement of a newborn mammal toward the nipple of its mother for the purpose of latching on to initiate breastfeeding. This movement uses the following reflexes: Babinski, Spinal Galant, Spinal Perez, amphibian, ATNR, and the Bauer crawl.
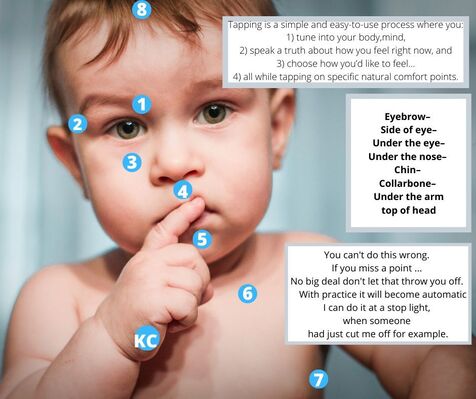
PAUSE: This is not just the golden hour where bonding between parent and baby is the priority, this is the moment after a busy period where the entire family can take a moment to process and take it all in. The story will be different for the birth person, parents, and for baby. •Routine procedures can wait! Emergency procedures are best done on the birthing parent with the cord attached whenever possible. (Raylene Phillips, Neonatologist, Loma Linda Medical Center, CA, USA) "When space is created to help the whole family’s experience be seen, heard, and felt, a new story of what happened can be experienced through connection." - Rebecca Thompson Hitt, MS, MFT Keep your baby with you. This is the period of trust versus mistrust, according to Erikson's. This is the period where baby really needs to be with their parents. It is important to not allow excessive crying during this period. A great method of keeping baby close and crying minimal is babywearing. There are studies called Why African Babies Don't Cry that explore the story of babywearing in African villages and how it allows babies to nurse on demand and constantly have the comfort of their parent. EFT Tapping: Emotional Freedom Technique Tapping is a great emotional regulation tool to teach infants and a great communication tool from parents to infants. It can be great to remind your baby that things are okay when you are feeling emotional. It can also be a great way to signal it is bedtime. Try incorporating this in your nightly routine around the time that you are changing your baby's diaper. Do some tapping just before bed and a foot massage, easy to offer while already lying down on the changing table. Both are great bonding exercises that touch reflexology points. Speak to your baby and hold healthy eye contact: Your baby communicates through the universal language of emotion. Our eyes hold much emotion. They are a way we recognize each other and a way that we show we are listening fully. When speaking with your baby practice holding eye contact. You can look them in the eyes and blink until they begin blinking in sync with you, a bonding exercise! Skin to skin, anytime! Skin to skin is not just important during immediate postpartum. It should be done well into the weeks following, between both parents. It is a great way too bond and should even be done during bottle feeds. During bottle feeds remember to alternate which side you are feeding on, the same way you would with the breast. Family Focused Stress Relief Sometimes whole family focused stress relief is extremely necessary when a parent is home all day and the other is not. The working parent may come home happy, but actually be bringing in more stress because they are not practicing family focused stress relief. The root prevention for this is setting up support systems. Where did your baby begin? With you and your partner and the love that you two share. When things do not feel solid we look at the roots. Sometimes the best place to connect is actually with your partner. If you are the birthing parent you may not understand the way your partner struggles to bond, but it is a struggle. Often times non gestational parents struggle to bond the same way the birthing parent does. This can happen in couples where neither parent is birthing the baby (adoption, surrogacy, etc). These feelings are normal and valid. Becoming parents is one of the two top ways to heal insecure attachment. You are a safe haven and secure base for your baby AND for your partner. I think it is important to remember here that so many bonding techniques for straight couples conceiving and birthing a baby do work for LGBTQIA+ community members and non gestational parents of any kind, as well.
One of the biggest things you can do for your infant to offer healing is talk to them. Tell them the story of how they came to be; egg and sperm origin, who carried their pregnancy, who was in the room when they came earthside, etc. Remind your infant of ways you connected with them. Did you pray for them? Did you speak to them even if you were not close by? How did you connect? Choosing differing routes for fertility can increase a baby's empathy: We learn empathy through these differing routes. When we see surrogates go through the journey of being a gestational carrier we see such great levels of empathy. I believe that level of empathy is being taught to baby in utero. When given the opportunity to speak to baby in utero, do it! Whether that opportunity is daily or monthly, do so. Tell them who you are, meet the 9 positive imprints mentioned above, and tell them what you will be doing to connect with them before you are physically in the same space again. In surrogacy, bonding with the surrogate is a great way to bond with baby as well. When interviewing surrogates remember to ask questions about meetings, communicating with baby, etc. You may want to be able to send voice messages knowing they will be played so that the baby can know you and your partner's voices. Keep your baby with you. This is the period of trust versus mistrust, according to Erikson's. This is the period where baby really needs to be with their parents. It is important to not allow excessive crying during this period. A great method of keeping baby close and crying minimal is babywearing. There are studies called Why African Babies Don't Cry that explore the story of babywearing in African villages and how it allows babies to nurse on demand and constantly have the comfort of their parent. EFT Tapping: Emotional Freedom Technique Tapping is a great emotional regulation tool to teach infants and a great communication tool from parents to infants. It can be great to remind your baby that things are okay when you are feeling emotional. It can also be a great way to signal it is bedtime. Try incorporating this in your nightly routine around the time that you are changing your baby's diaper. Do some tapping just before bed and a foot massage, easy to offer while already lying down on the changing table. Both are great bonding exercises that touch reflexology points. Speak to your baby and hold healthy eye contact: Your baby communicates through the universal language of emotion. Our eyes hold much emotion. They are a way we recognize each other and a way that we show we are listening fully. When speaking with your baby practice holding eye contact. You can look them in the eyes and blink until they begin blinking in sync with you, a bonding exercise! Skin to skin, anytime! Skin to skin is not just important during immediate postpartum. It should be done well into the weeks following, between both parents. It is a great way too bond and should even be done during bottle feeds. During bottle feeds remember to alternate which side you are feeding on, the same way you would with the breast. Family Focused Stress Relief In couples where one person is a birthing parent, but the other is not I think that whole family bonding practices are very important. This allows for there to feel like less of a hierarchy when it comes to one on one bonding. This also allows for whole family stress relief. Sometimes whole family focused stress relief is extremely necessary when a parent is home all day and the other is not. The working parent may come home happy, but actually be bringing in more stress because they are not practicing family focused stress relief. The root prevention for this is setting up support systems. This is important with one birthing parents or none. One on One Time One of the biggest recommendations I have for new parents is for the working parent to set up one on one time with the baby. This allows bonding and allows them to care for their partner. Their partner can get to bed early or take some alone time while the working partner is caring for baby. This could be a hour in the evening just to help with the bedtime routine. Snuggles, stories, and the final feeding done by the working parent while the birthing parent rests or takes a sitz bath. Maybe afterwards you eat dinner together if baby is asleep and the gestational parent is awake? Find a routine that works for your family and allows bonding between all parties. By caring for ourselves we care for others indirectly, what will that look like for your family? We can learn secure attachment, it does not have to happen prenatally AND you could be healing your own insecure attachment while pregnant through the work you are doing for your baby.
The light isn't green forever. AuthorJess Kimball is a Full Spectrum Doula and Certified Lactation Counselor trained in Ayurvedic and Chinese medicine. |
||||||||||
|
EST. 2016
North Carolina | Vermont Jess Kimball |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
Jess Kimball provides doula care, birth photography, and a variety of other services to families!
|



 RSS Feed
RSS Feed