|
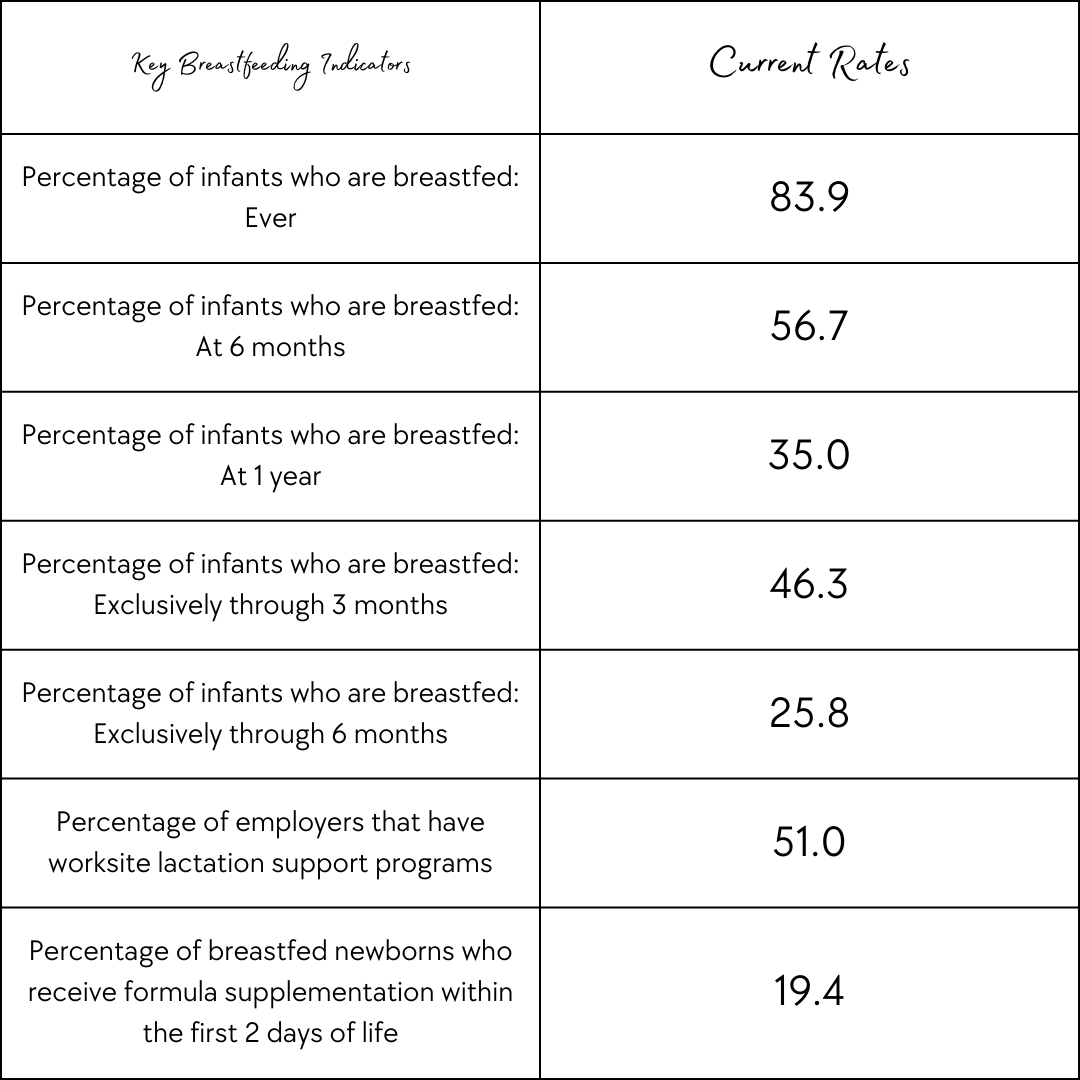
What started as a scientific campaign to promote the research showing that breastmilk is the best option for infants has now turned into an intense pressure that leaves parents who cannot or choose not to breastfeed feeling ashamed and inadequate. “Breast is Best” is the notion held by many organizations parents and providers respect, like the World Health Organization. The goal was to inform expectant parents of the benefits of exclusive breastfeeding. Exclusive breastfeeding is breastfeeding as the only form of feeding for at least the first six months of life. This campaign started in the 1960s or 70s, although the exact origin is still unknown. The campaign has normalized breastfeeding in public and increased rates of families attempting to breastfeed. People feel empowered to pump at work and advocate for their rights around lactation and the workplace. Some of the benefits of breastfeeding include that the nutrients of breastmilk are better absorbed by your baby and are the best to support brain and nervous system development. Certain fats in breast milk help with eyesight. Breastfeeding lowers the risk of SIDS (sudden infant death syndrome) and helps strengthen a baby’s immune system, but how many people stick with breastfeeding when they leave the hospital? How many people actually exclusively breastfeed? There are many things that impact the rate of parents breastfeeding. Some parents simply do not have the option because they do not lactate. Others want to, but struggle because of barriers making it hard to access lactation support or make breastfeeding a sustainable option long term. We have come a far way with workplace breastfeeding and pumping rights, but we still have a long way to go. What are the barriers to breastfeeding? One of the biggest reasons parents choose not to breastfeed is because of a barrier in place. In most cases, a decision not to breastfeed has a reason behind it. Barriers can include lack of knowledge, societal norms, lack of support, employment and child care, barriers to health services, and various lactation problems. While the “Breast is Best” campaign did increase education it did not remove all of these barriers. Even without all of these barriers it comes down to something really simple, it is the parents' choice if they want to breastfeed, bottle-feed pumped milk, or use formula. The first recommendation from the American College of Obstetricians and Gynecologists (ACOG) is that “Parents have the right to make their own informed choice about whether or not to breastfeed”. Providers are meant to provide unbiased non-coerced support. Despite this recommendation, many parents still feel like they do not have a choice. When they cannot breastfeed they feel like they are letting their baby down. Breastfeeding May Better Your Mental Health, But The Pressure to Breastfeed Does Not Breastfeeding supports hormonal processes that induce the release of oxytocin. Oxytocin helps with parent-infant bonding and lowers cortisol levels. Cortisol is the stress hormone and higher rates lead to mental health problems. Breastfeeding parents are more likely to report positive mood, less anxiety, and increased calm according to Frontiers in Global Women’s Health, but it is not reported how many months into breastfeeding the parents in this report were. The pressure to breastfeed begins far before the baby arrives. The decision to breastfeed is typically made before or during pregnancy. It is something a lot of parents think about when trying to conceive. Parents research the best pump, best chair to nurse in, and most comfortable nursing bras. By just three months less than half of the babies in the U.S. are breastfed exclusively. This drops to 25% by six months. Despite this, there is still intense pressure to breastfeed that takes a huge toll on parents' mental health. The pressure comes from health care providers, some of which do not even choose to breastfeed their children. It comes from lactation consultants and even from other moms who think they know best for every mom. The truth is, they don’t. Only you can decide if breastfeeding works for your family and that decision may change over time. When beginning your breastfeeding journey it may start rocky and improve or it may start great and take a toll on you later. It may be a combination of things taking a toll whether that is lack of sleep catching up to you or something else. Only you know your body and your mind, and you know when you have reached your limit. All of those voices telling you what they believe you should do for your baby can take a toll. From Facebook groups to online forums to moms at playgroups, people love to try to tell other parents how to parent. The psychological pressure to breastfeed can increase the risk of postpartum depression. The feeling that you are unable to reach the goal you set for yourself can feel very defeating. That feeling may contribute to postpartum depression and other postpartum mood and anxiety disorder symptoms. Nursing For Women's Health released a piece supporting the idea that more research is needed on what the pressure to breastfeed is doing to the mental health of parents. The signs of mental health decline could include feelings of sadness, anxiety, fear, trouble sleeping, anger, or irritability. More information on postpartum mood and anxiety disorders (PMADS) can be found here. While this research may currently be limited, many parents are still speaking out about the way this pressure has affected them personally. Recent trends in childbirth can even impact the success of breastfeeding despite so many hospitals being part of the “baby-friendly hospital initiative”. This initiative supports early initiation of breastfeeding, skin to skin, delayed cord clamping, and more parent-baby bonding techniques, but providers following this method have been reported of holding formula hostage when families request it and ignoring the recommendation by the ACOG that parents have a unique perspective and know what is right for their baby. What if I can’t breastfeed? We live in a world with a lot of options and those options are becoming more and more accessible as this discussion on the reality of breastfeeding becomes more discussed. If providing your baby with breastmilk is important to you you may be able to pump or try donor milk. You may decide the formula in combination with breastmilk works best for your family or you may choose to exclusively feed your baby formula. There are many options when it comes to formula because just like breastfeeding there is no one option that works for everyone. When exploring formula options you can find a variety of brands and a variety of recipes within each brand. Some formula recipes are designed to support a sensitive stomach or designed for premature babies. If you are choosing formula; just like deciding what feeding option you will use, you will decide which formula type is best for your baby. At the end of the day, the most important thing is that your baby is fed and that you are not pouring from an empty cup. A fed baby is a healthy baby. “Fed is Best” is a movement to help normalize all feeding options. The goal is to remind parents that what is healthy is that their baby is fed. The organization offers various resources to avoid harm to the physical health of infants who need the formula and the mental health of parents being pressured to breastfeed. Remember, to avoid pouring from an empty cup you need to care for yourself. Breastmilk may be ideal for each infant, but it is not always ideal for each parent. The “Breast is Best'' movement should not only increase education but also strive to break down barriers to breastfeeding for those who wish to breastfeed. As a society, we should strive to create an inclusive community for parents that offers empathy and understanding when a parent decides to do something healthy for their family but is not a choice we would have made ourselves. Each family is different, but so is each baby. What worked with one may not work for your next. References:
C. D. C. (2021, November 24). Breastfeeding report card. Centers for Disease Control and Prevention. Retrieved February 13, 2022, from https://www.cdc.gov/breastfeeding/data/reportcard.htm C. D. C. (2021, August 24). Facts. Centers for Disease Control and Prevention. Retrieved February 13, 2022, from https://www.cdc.gov/breastfeeding/data/facts.html J, H. (n.d.). Breast milk is best. Johns Hopkins Medicine. Retrieved February 13, 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/breastfeeding-your-baby/breast-milk-is-the-best-milk Office of the Surgeon General (US). (1970, January 1). Barriers to breastfeeding in the United States. The Surgeon General's Call to Action to Support Breastfeeding. Retrieved February 13, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK52688
0 Comments
Leave a Reply.The light isn't green forever. AuthorJess Kimball is a Full Spectrum Doula and Certified Lactation Counselor trained in Ayurvedic and Chinese medicine. |
|
EST. 2016
North Carolina | Vermont Jess Kimball |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
Jess Kimball provides doula care, birth photography, and a variety of other services to families!
|
 RSS Feed
RSS Feed