|
Basics of Babywearing Babywearing is a practice that has been around for years and years. Babywearing took a mainstream turn in the 1960s when the Snugli baby carrier was invented. Peace Corp volunteers in Togo, West Africa were inspired by the way mothers wore their babies. Ever since then it seems there are a million different options when it comes to which types of carriers to purchase. Babywearing Positioning If you choose to babywear, it is important to practice babywearing safety with carrying. One key safety tip: babies should always be positioned in a way that they are not breathing in the same air, with baby's head and baby's face turned to the side. Be cautious of how baby's legs are positioned also. Baby’s thighs should spread around your torso with their knees bent slightly higher than their bottom. Always check to see if your carrier is approved by the international hip dysplasia institute. Baby should not face outward until they’re 6 months old with strong head and neck control, and structured carriers should only be used for infants over 7 pounds. Benefits of Babywearing Babywearing is a great way to multitask. A baby wearer gets to be hands free, which is one of the many benefits of babywearing. So whether you’re cooking dinner, running errands, or double wearing multiples, babywearing is extremely helpful! A few of the other benefits of babywearing include:
Slings The sling is a one shoulder carry great for small babies into toddlerhood. I personally love the ring sling. It is very quick and convenient once you get the hang of it. A few favorite ring slings are designed by Aloha and Light and WildBird. With newborns, a snug front carry is preferred and with babies over five months, more of a hip carry works better. Toddlers may enjoy the back carry more and you will probably find it much more comfortable for that age! Ring slings are super compact and probably the easiest carrier to toss in the diaper bag. Wraps: Woven vs Stretchy I love a stretchy wrap (like the Moby wrap, Boba or Baby K'tan), but in my experience as a babywearing educator, people with heavier babies tend to like the structure of the woven wraps more. The stretchy wrap is extremely comfortable and feels like a second layer of clothes when worn. There are tons of ways to wrap and it can seem intimidating at first, but the learning curve isn't high. Once you find your favorite wrap style it’s easy to just stick with that and really enjoy the wrap life! Wraps are similar to a long piece of fabric, and tend to be quite long, usually about 18 feet. I recommend wrapping before getting in the car to go somewhere. That way it is ready for the baby upon arrival at our destination! Mei Tai These carriers are soft material with a structured back panel. Straps are pulled around the waist and other the shoulder, then tied into a secure knot. They are versatile and can be tied in more ways than a sling, but not as many as a wrap. They can be used with all ages, are convenient, not super bulky, and quite comfortable. Soft Structured Carriers This type of carrier, also known as an SSC, has a structured seat, padded shoulder straps, and buckles on the back and waist. They are quick to put on, but may require an extra set of hands to help buckle or adjust. My personal favorite is the Lillebaby because of the amazing back support (but Ergobaby, Baby Bjorn and Beco also make great soft structured carriers). These carriers also typically come with attachments like infant inserts and sunguards! Onbu The onbuhimo is meant for infants sitting independently up to toddlerhood. It is extremely easy to put on and doesn’t involve any kind of waistband. It is a Japanese style carrier with a chest belt. The style is similar to a backpack, but can be used to front carry. Back carries tend to be more comfortable all around. If you do choose to babywear, be sure to take your carrier with you on the go - just as you would your car seat and stroller. You never know when babywearing will come in handy! Happy Babywearing!
0 Comments
Oxytocin2/4/2023 Hormones play a massive role in how you feel postpartum, bonding with your baby, and how your body heals. Cortisol is the hormone that rises with stress. Dopamine and serotonin are the hormones that make us feel happy. Oxytocin is the one responsible for that warm feeling we get inside when we see someone we love. Oxytocin is produced in the hypothalamus and released during sex, childbirth, and lactation to aid reproductive functions. It has physical and psychological effects, including influencing our social behavior and emotion! Small amounts of oxytocin are passed through milk to the baby along with other hormones such as melatonin, which aids in sleep regulation. What is oxytocin?Oxytocin is commonly referred to as the “love drug” because it is released during childbirth, breastfeeding, sex, and physical touch. It is higher in women because it is key in childbirth! Oxytocin is associated with empathy and trust. Oxytocin increases during orgasm, hugging, breastfeeding, and when you smell a newborn baby. An increase in oxytocin usually makes you feel warm and fuzzy inside! Synthetic Form: PitocinPitocin is the synthetic version of oxytocin. It is used during labor and immediately postpartum to induce contractions. This can induce labor or, when used postpartum, can treat a hemorrhage. Once administered for an induction its chemical process begins in about thirty minutes, although labor may last many hours. Sometimes Pitocin is also used to help with stalled labor, an intervention before something more invasive, such as a cesarean section, is recommended. Natural Flow:In Pregnancy Increased oxytocin levels affect metabolism. This helps a pregnant person gain weight and store energy for times of rapid fetal growth. During the third trimester, oxytocin increases caution, helping the pregnant person protect themself and practice better spatial awareness. Childbirth and Immediately Postpartum Oxytocin is responsible for contractions in labor and postpartum. There is an oxytocin release after birth that causes your senses to be intensified. This allows you to connect with the smell and feel of your baby, and them with yours. You may hear the term “golden hour” to describe the hour after birth when oxytocin flow and skin to skin is so important. Breastfeeding Oxytocin is responsible for the letdown reflex when nursing. This increased oxytocin flow during nursing allows the uterus to continue contracting and heal postpartum. It begins flowing as soon as the parent expects a feeding and again when the baby begins suckling. Prolactin is ultimately what causes milk production, but oxytocin is what gets the milk flowing! Without oxytocin, milk wouldn’t flow so easily and it would be harder for babies to nurse. Increasing your oxytocin flow could improve your breastfeeding experience! Sex Throughout sexual activity, and especially during orgasm, oxytocin is released by both partners. This strengthens the connection between you and your partner and typically results in you wanting to spend more time with them! The Newborn Baby Smell The newborn baby smell sets off the same receptors in the brain that drugs set off. The newborn baby smell is addicting! When mothers and nonmothers smelt baby clothes in a study (reported by the Smithsonian Magazine), MRI showed the parts of the brain associated with reward learning lighting up. The dopamine surge that occurred is associated with sexual and drug-type cravings. The reaction appeared to be stronger in mothers and was similar to the reaction we see in patients using mental health drugs. This reaction is a result of evolution! Bonding is essential for the survival of an infant. Benefits1. Parent-Baby Bonding! Oxytocin is vital in bonding between a parent and baby, especially during the first hour postpartum, the golden hour! 2. Success in nursing! The oxytocin increase while breastfeeding can help postpartum parents' mental health, making them more eager to breastfeed. Oxytocin can boost your mental health, which helps with the stress of breastfeeding and the pressure others parents may be putting on you. 3. Stress Relief! Oxytocin lowers blood pressure and cortisol levels! A great boost for your mental health during the baby blues and times when parents are at higher risk of postpartum mood and anxiety disorders (PMADs). 4. Increased Pain Tolerance! Ina May Gaskin once said that the best way to get a baby out is the way you got it in! Oxytocin increases pain tolerance, but also helps ease pain in labor. Nipple stimulation and kissing your partner, along with other ways of expressing love, have been proven to reduce pain in labor and even help labor progress when it appears to be stalled. That connection with your partner helps fear subside so the psychological blocks you may have are removed. That combined with oxytocin flow helping with contractions allows labor to move along more seamlessly! 5. Better sleep! Oxytocin leaves you feeling calm and tranquil, this typically results in much better sleep! This is especially important in pregnancy and postpartum. So much growth is happening in pregnancy, rest is vital to your body! Lack of sleep postpartum can increase the risk of PMADs. Babies also tend to sync their breathing to the caregiver in the room, this is part of why room sharing can reduce the risk of sudden infant death syndrome (SIDS). When you are sleeping better and your breathing is calm, your baby will sleep better too. Increase Oxytocin Through BondingHow do you do this? Skin to skin! When you spend time having skin-to-skin contact with your baby you are increasing your oxytocin. Taking time to smell your baby’s head and become familiar with how they smell and feel, and allowing them the same opportunity to become familiar with you, is the ultimate way to increase oxytocin and strengthen the bond between you and your baby! Skin to skin can be done while resting in bed, while nursing, or even while babywearing. You can babywear topless and place a large cardigan or zip-up hoodie over the carrier to stay warm. This is most comfortable with a cotton wrap or cloth carrier. Skin to skin can also happen when co-bathing! As long as you feel comfortable bathing with your baby, they are not getting their umbilical stump wet, you have an extra set of hands, and you have been cleared by your doctor to take baths…co-bathing is a go! You can sit in a warm bath with your baby on your chest or with your legs bent and your baby more in your lap. This is a great way to get your baby used to bath time and get that skin-to-skin time! Just make sure you have someone close by in case you need them to take the baby so you can get out of the bath easier. Wet babies are very slippery, like a little wet seal! You can also lay a towel on top of a bath mat next to the tub and gently place your baby on the towel to wrap them before you step out. As long as there are no small items for a baby to grab or anything that may step on the baby, like an over-excited dog, babies are typically very safe lying on the floor. It’s best to exit the tub hands-free and this is a good way to do so if you don’t have someone to lend a hand. Oxytocin is an extremely important and interesting hormone responsible for the way the feeling of love is expressed inside our bodies! It can make a huge difference in how labor goes for a birthing parent, the attachment between caregiver and baby, and the experience of nursing for both parent and baby! Increasing oxytocin can enhance your experience as a parent, your relationship with your partner, and your overall mental health! References:
Magazine, S. (2013, September 24). The smell of newborn babies triggers the same reward centers as drugs. Smithsonian.com. Retrieved February 19, 2022, from https://www.smithsonianmag.com/smart-news/the-smell-of-newborn-babies-triggers-the-same-reward-centers-as-drugs-58482/ McKenna, J. J. (n.d.). Babies need their mothers beside them. Babies Need Their Mothers Beside Them - The Natural Child Project. Retrieved February 20, 2022, from https://www.naturalchild.org/articles/james_mckenna/babies_need.html Uvnas-Moberg K, Petersson M. Oxytocin, ein Vermittler von Antistress, Wohlbefinden, sozialer Interaktion, Wachstum und Heilung [Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing]. Z Psychosom Med Psychother. 2005;51(1):57-80. German. doi: 10.13109/zptm.2005.51.1.57. PMID: 15834840. Whitley J, Wouk K, Bauer AE, Grewen K, Gottfredson NC, Meltzer-Brody S, Propper C, Mills-Koonce R, Pearson B, Stuebe A. Oxytocin during breastfeeding and maternal mood symptoms. Psychoneuroendocrinology. 2020 Mar;113:104581. doi: 10.1016/j.psyneuen.2019.104581. Epub 2019 Dec 31. PMID: 31911347; PMCID: PMC8117182. From hair loss to night sweats, postpartum is no joke. Oftentimes postpartum symptoms go unspoken about, leaving women shocked, scared, and unprepared when normal, common symptoms arise. One of the least talked about parts of postpartum is vaginal dryness. This is common, normal, and continues well beyond six weeks postpartum. Vaginal dryness can cause irritation, burning, and pain with intercourse. It can be accompanied by a dry vulva as well. Around 43% of postpartum women experience vaginal dryness. And we need to talk about it more; because talking about it allows people to prepare for it! What causes postpartum vaginal dryness? Postpartum vaginal dryness is caused by hormonal changes. Estrogen and progesterone trigger puberty and they also cause the buildup of a lining in your uterus during your menstrual cycle. If a fertilized egg isn’t implanted in this lining, estrogen and progesterone levels drop, and the uterine lining is shed as your period. Estrogen is a hormone that helps maintain the vagina’s lubrication, elasticity, and thickness. These levels increase throughout pregnancy. As the placenta forms it begins producing these hormones as well! After giving birth these levels rapidly decline. Within 24 hours of giving birth estrogen and progesterone are back at their pre-pregnancy levels. The increase in estrogen during pregnancy enables the uterus and placenta to improve vascularization (the formation of blood vessels), transfer nutrients, and support the developing baby. The rapid increase in estrogen levels during the first trimester may cause nausea. During the second trimester, it plays a major role in the milk duct development that enlarges the breasts. What symptoms occur when experiencing vaginal dryness? Inability to maintain lubrication during sex; burning, discomfort, or itching in the vagina; painful urination due to irritation of vaginal tissue; dryness during intercourse and difficulty inserting tampons; and increased frequency of urinary tract infections (UTIs) are common symptoms of vaginal dryness. Estrogen levels can also drop because of:
Breastfeeding: Normal estrogen levels are what help maintain the tissues of the vagina. Low levels seen in breastfeeding can mimic the decreased hormone levels seen in menopause. This can result in thinning of the skin and increased vaginal dryness, the same way postmenopausal women experience this. All women have low levels of estrogen for the first couple of months after giving birth. Continued breastfeeding extends this period for at least six months and for some women the lower levels may last as long as they are breastfeeding. Milk volume may decrease with the use of estrogen; however, no detrimental effects have been shown on infant growth or development. Postpartum thyroiditis: Postpartum vaginal dryness can also be caused by postpartum thyroiditis. This is an inflammation of the thyroid gland. The thyroid produces hormones that are vital to various bodily functions, including metabolism, but sometimes these hormones become imbalanced. Postpartum thyroiditis affects up to 10% of postpartum women. For an overproducing thyroid, your doctor may suggest beta-blockers to help reduce symptoms, or your doctor may recommend thyroid hormone replacement therapy for an under producing thyroid. Symptoms include:
Many changes throughout pregnancy and childbirth change sex for couples. While most mothers are cleared at 6 weeks to resume sexual activty it is important to remember that this is strictly from an infection risk standpoint. You may not feel ready at 6 weeks and your partner should be aware that most women are not ready at that point! Educating your partner can help reduce the pressure you feel to resume sexual activity. Vaginal dryness can make sex uncomfortable and cause small tears during intercourse. This is because without enough estrogen, not only will you not have the same level of moisture, your vaginal tissue can shrink and become thinner. When you do feel ready to resume sexual activity keep these tools in your toolkit:
“If you are concerned about sex being painful, you can seek out pain relief options before having sex, such as a warm bath or an over-the-counter pain reliever. Using a lubricant is also recommended to combat vaginal dryness and make sex more comfortable. Relax, take it slow and communicate with your partner what does and does not feel good in order to make the experience a positive one. You can also consider other forms of sexual intimacy – such as massage or oral sex – as alternatives to vaginal intercourse.” How to handle vaginal dryness? Some women choose to take an estrogen supplement, but these do increase the risk of cancer and blood clots. Three types of vaginal estrogen:
What other vaginal changes occur postpartum? A person can expect vaginal changes after giving birth. It can take anywhere from 12 weeks to a year for your vagina to go back to its pre-birth state. Common changes include perineal pain, pain during sex, bleeding, and vaginal dryness as well as:
If you feel ready and are cleared by your provider try having sex, and have lots of lube handy! But remember that you can stop at any point. Communication during sex is not a mood-killer! Let your partner know what is working and what isn’t, and have fun! References:
Kelsey JJ. Hormonal contraception and lactation. J Hum Lact. 1996 Dec;12(4):315-8. doi: 10.1177/089033449601200419. PMID: 9025449. UHBlog. (2022, February 24). Sex after birth: Resuming sexual intimacy after having a baby. University Hospitals. Retrieved May 23, 2022, from https://www.uhhospitals.org/Healthy-at-UH/articles/2022/02/sex-after-birth-resuming-sexual-intimacy-after-having-a-baby The Psychology of Childbirth2/4/2023 Throughout pregnancy and postpartum women are constantly warned about the physical changes their body will experience. We have talked more and more about PMADs (perinatal mood and anxiety disorders) recently, but what about the psychological changes that occur during childbirth? Some women describe childbirth as a euphoric feeling that leaves them immediately wanting to do it again while others describe the opposite. Psychological research on childbirth is rare, even though research from other scientific fields such as obstetrics or midwifery highlights the importance of psychological factors in childbirth. Limited research we do have is showing that psychological state during childbirth can also impact infant behavior patterns. Throughout Labor...In the day or two before you go into labour, you may notice heightened anxiety, mood swings, weepiness, or a general sense of impatience. This may not be entirely noticeable due to other hormonal fluctuations that are occurring. Labor and birth entail physical and psychological challenges such as coping with pain, loss of control, and possibly medical interventions. Birth affirmations are a powerful way to help anchor yourself in your mind. Keeping a “birth mindset” may be a beneficial way to promote a positive psychological birthing experience. Some affirmations include:
Your Birth TeamThe people you surround yourself with make a difference too. A study found that the people attending the birth greatly impacted the birthing persons psychological state, “Women’s psychological experience of physiological childbirth is strongly influenced by the people present at their birth. Women indicated that close relatives, mostly their partner and mother, as well as care providers were highly relevant for the way women experienced their birthing process. Women described the presence of their partner as the person with whom they most closely shared their experience and relied on for support, confirming that human birth is a social event. This is consistent with other studies that emphasised the decisive contribution partners can make to feelings of trust and the woman’s wish for a physiological birth. Women indicated the midwife’s presence as being critically important. At the beginning of the labour, women tended to want to be alone and at a distance from the midwife, but, as labour intensified, they wanted the midwife to be more visible and present while supporting the woman’s control, or taking control if women wanted to hand it over.” This study indicates that women are more likely to experience a psychologically positive physiological birth when they feel that a supportive and compassionate companion or healthcare provider is by their side, and is very sensitive and attentive to their cues. Hormones play a huge role in the psychology of birth as well.Oxytocin is the one we hear about most often because it is released in the highest doses throughout childbirth and breastfeeding. Oxytocin is responsible for contractions in labor and postpartum. There is an oxytocin release after birth that causes your senses to be intensified. This allows you to connect with the smell and feel of your baby, and them with yours. Oxytocin is responsible for the letdown reflex when nursing. This increased oxytocin flow during nursing allows the uterus to continue contracting and heal postpartum. Oxytocin is responsible for that euphoric feeling many people with a positive birthing experience describe. It is a stress reliever and helps lower blood pressure and cortisol levels in labor. Endorphins are another important hormone throughout labor! For women who don’t use pain medication during labor, the level of endorphins continues to rise steadily and steeply through the birth of the baby. High endorphin levels during labor and birth can produce an altered state of consciousness that can help a woman through labor even if it is a long labor. High endorphin levels can make you feel alert, attentive and even euphoric (theres that word again!). Approaches to ChildbirthDick-Read Method: Grantley Dick-Read was an English obstetrician and pioneer of prepared childbirth in the 1930s. In his book Childbirth Without Fear, he suggests that the fear of childbirth increases tension and make the process of childbearing more painful. He believed that if mothers were educated, the fear and tension would be reduced and the need for medication could frequently be eliminated. The Dick-Read method emphasized the use of relaxation and proper breathing with contractions as well as family support and education. Lamaze Method: The Lamaze method originated in Russia and was brought to the United States in the 1950s by Fernand Lamaze. The emphasis of this method is on teaching the woman to be in control in the process of delivery. It includes learning muscle relaxation, breathing though contractions, having a focal point during contractions and having a support person who goes through the training process with the mother and serves as a coach during delivery. LeBoyer: The Leboyer Method of “Gentle Birthing” involves giving birth in a quiet, dimly lit room and allowing the newborn to lie on the mother’s stomach with the umbilical cord intact for several minutes while being given a warm bath. Beyond BirthA study found that the psychological state of the mother during childbirth helped predict behavioral challenges in infancy. Social support enhanced the mother’s childbirth experience, benefitting her perceptions of her baby’s early temperament. These findings further support current World Health Organization guidelines (2018) on the importance of making childbirth a ‘positive experience’ for women. Certain obstetric interventions, such as assisted birth, have been directly associated with increased levels of neonatal cortisol and crying (Taylor et al., 2000; Gitau et al., 2001). Newborn infants up to 8 weeks are more likely to be unsettled after an assisted birth or emergency C-section (Taylor et al., 2000; Gitau et al., 2001). Some have suggested that birth complications could affect longer term infant temperament due to the subsequent increase in maternal and foetal cortisol levels. Perinatal or postpartum mood and anxiety disorder (PMAD) is the term used to describe distressing feelings that occur during pregnancy (perinatal) and throughout the first year after pregnancy (postpartum). PMADs can develop in the postpartum period from a traumatic birth experience. A negatively perceived birth experience can have a negative impact on the mother–child interaction even months after birth (Durik et al., 2000) and on the occurrence of postpartum depression (Bell & Andersson, 2016). The TakeawayFor the best chance of a positive psychological birth experience a birthing person should do the following:
References:
Olza, I., Leahy-Warren, P., Benyamini, Y., Kazmierczak, M., Karlsdottir, S. I., Spyridou, A., Crespo-Mirasol, E., Takács, L., Hall, P. J., Murphy, M., Jonsdottir, S. S., Downe, S., & Nieuwenhuijze, M. J. (2018, October 1). Women's psychological experiences of physiological childbirth: A meta-synthesis. BMJ Open. Retrieved May 22, 2022, from https://bmjopen.bmj.com/content/8/10/e020347 In 2022 one in eight women still report symptoms of maternal depression. Rates of PMADs are on the rise and we are finally beginning to discuss this more! As the media begins to shed light on this ever so important topic we are also shedding light on the glaring disparities in maternal mental health. There has been a huge focus lately on maternal morbidity and the large gaps we see between white patient outcomes and black, indigenous, and people of color (BIPOC) outcomes, but there is room for an even bigger discussion; the discussion of disparities across all parts of maternal health. PMADs are just one example of another maternal health category that shows disparities by race. Perinatal or postpartum mood and anxiety disorder (PMAD) is the term used to describe distressing feelings that occur during pregnancy (perinatal) and throughout the first year after pregnancy (postpartum). When it comes to PMADs, African American women have a higher risk of developing perinatal depression compared to white women, Latina women also have a higher risk. Current research from the Icahn School of Medicine at Mount Sinai found that 44% of African Americans reported depressive symptoms two weeks after delivery, compared to 31% percent of white women. Despite a higher rate of cases in BIPOC parents, Black and Hispanic women are less likely than White women to be diagnosed with and receive treatment for postpartum depression. Structural racism causes significant inequities in the diagnosis of perinatal and maternal mental health disorders and access to perinatal and maternal mental health treatment. Improving racial equity in healthcare, increasing screening for PMADs, and increasing community support could greatly improve maternal mental health outcomes. What is Racial Equity? The Center for Law and Social Policy (CLASP) defines racial equity as the condition that would be achieved if your racial identity no longer predicted how you fare in life. The Center for Social Inclusion (CSI) states that: “when we achieve racial equity: People, including people of color, are owners, planners, and decision makers in the systems that govern their lives. We acknowledge and account for past and current inequities, and provide all people, particularly those most impacted by racial inequities, the infrastructure needed to thrive.” Improving racial equity would drastically lower disparities in maternal health. Screening for Maternal Mental Health Concerns: A study found disparities between likelihood to receive PMAD screening and race. Clinic site was the strongest predictor of screening, accounting for 23–30% of the variability in screening prevalence. After adjusting for clinic, women who were BIPOC were less likely to be screened postpartum than white women). Those insured by Medicaid were also less likely to be screened. Social determinants of health prevent many people from racial and ethnic minority groups from having fair opportunities for economic, physical, and emotional health. Maternal Mental Health Disparity Statistics:
Upstream Approach: Using upstream approaches to health and racial equity, such as addressing the conditions where people live, work, and play that influence their health. Many community resources that are known to lower rates of PMADs are not accessible to low income families, such as doula care. The push for doulas to be covered by insurance and Medicaid is one way we can make doula care more accessible. Many states are using grant funding to implement mental health resources and training courses to combat the maternal mental health crisis. Vermont implemented STAMPP. Diversity in the Workplace: Diversity in health care helps ensure all backgrounds, beliefs, ethnicities, and perspectives are adequately represented in the medical field. Studies have found that patients are more likely to trust and open up to providers that look similar to them. It has also been proven that a diverse workplace minimizes biases that hurt BIPOC patients and create negative outcomes for BIPOC patients. Healthcare providers should learn how to recognize unconscious bias in themselves and in their office, address any concerns patients may have, and provide all patients with respectful care. All healthcare providers should prioritize continuing education on racial disparities and cultural competency. States and communities can prioritize identifying and addressing social factors influencing; maternal health such as unstable housing, transportation access, food insecurity, substance use, violence, and racial and economic inequality. Other important methods of improvement include: valuing, honoring, and investing in community and traditional healing practices; and promoting integrated care and shared decision making. Resources aiming to prevent and reduce racial disparities:
References:
Goyal, D., Gay, C., & Lee, K. A. (2010). How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers?. Women's health issues : official publication of the Jacobs Institute of Women's Health, 20(2), 96–104. https://doi.org/10.1016/j.whi.2009.11.003 Hartwell M, Lin V, Gatewood A, Sajjadi NB, Garrett M, Reddy AK, Greiner B, Price J. Health disparities, COVID-19, and maternal and childbirth outcomes: a meta-epidemiological study of equity reporting in systematic reviews. J Matern Fetal Neonatal Med. 2022 Mar 13:1-9. doi: 10.1080/14767058.2022.2049750. Epub ahead of print. PMID: 35282754. Saluja B, Bryant Z. How Implicit Bias Contributes to Racial Disparities in Maternal Morbidity and Mortality in the United States. J Womens Health (Larchmt). 2021 Feb;30(2):270-273. doi: 10.1089/jwh.2020.8874. Epub 2020 Nov 25. PMID: 33237843. PMADs, What are they?2/4/2023 Let’s start by defining PMADs: Perinatal or postpartum mood and anxiety disorder (PMAD) is the term used to describe distressing feelings that occur during pregnancy (perinatal) and throughout the first year after pregnancy (postpartum). This is different from baby blues. Around 50 percent to 80 percent of new mothers experience mood swings during the first two to three weeks after giving birth. This is referred to as the “baby blues”. Symptoms of a perinatal or postpartum mood disorder occur daily for more than two weeks. If you believe you are experiencing PMADs please reach out to a healthcare provider or, if necessary, call 911 for emergency help. Symptoms of a mood disorder:
Types of PMADs: Perinatal or postpartum depression: Depression that occurs after childbirth. Symptoms might include insomnia, loss of appetite, intense irritability, and difficulty bonding with the baby. Treatment may include counseling or medication. Perinatal or postpartum anxiety disorder: 10 percent of pregnant and postpartum women experience significant anxiety symptoms. Symptoms include
Perinatal or postpartum psychosis: One in 1,000 suffer a rare and severe form of a mood disorder called perinatal or postpartum psychosis.Those who have been diagnosed with a bipolar disorder, schizophrenia or other psychiatric challenges may have a higher risk for developing this form of mood disorder. Women who have experienced perinatal or postpartum psychosis in the past have a 30 percent to 50 percent recurrence risk. Symptoms include:
Perinatal or postpartum obsessive-compulsive disorder (OCD): OCD is an often misunderstood and misdiagnosed disorder that affects as many as 3 percent to 5 percent of new mothers and even some new fathers.Risk factors include a personal or family history of anxiety or OCD. More than 38 percent of women with OCD also struggle with an underlying mood disorder.Intrusive thoughts and images are the most common symptoms. Research has shown that these images are driven by anxiety and not psychosis. Other symptoms may include:
PMAD Statistics:
Effects on baby: If left untreated, PMADs adversely affect parental cognitions and beliefs, attachment to the infant, and the growing caregiver-infant relationship. PMADs affect early developmental outcomes of infants including neurosynaptic development, regulatory development, and developmental milestones.PMADs can lead to premature birth, risk of SIDs, and a need for neurodevelopmental or neurobehavioral support. Research shows that depressed and anxious parents often smile less, talk less, and are less likely to touch or engage with their newborns throughout the first year of life. Children of parents with depression and anxiety may develop learning, attention or behavioral difficulties as they grow older. Older children may also suffer from the loss of maternal/paternal attention and support, and they may become depressed or anxious as teenagers. Endocannabinoids and PMADs: Endocannabinoids are responsible for helping regulate various processes, such as pain, memory, mood, immunity, and stress. The endocannabinoid system is known to have positive effects on depression. One way to improve mental health is exercise. Intense exercise increases circulating endocannabinoid. Including exercise in your routine can help combat PMADs and baby blues. A study published in the British Journal of Sports Medicine found that endurance exercise increases the level of endocannabinoids in the body. These substances have an effect similar to the active ingredient in marijuana. Another way to reinforce endocannabinoids is through food. Endocannabnoid reinforcing foods include: Hemp seeds and oil, chia seeds, walnuts, flax seeds and oils, eggs, sardines and anchovies. Essential fatty acids, chocolate, herbs, spices, and tea can also naturally stimulate the endocannabinoid system (ECS). The ECS is involved in reconsolidation and extinction of the fear memory in the fear memory paradigms as well as in anxiety. Endocannabinoid signaling may ensure an appropriate reaction to stressful events. Including ECS reinforcement in your postpartum plan could be extremely beneficial! Disparities in PMADs: African American women have a higher risk of developing perinatal depression compared to white women, Latina women also have a higher risk. Current research from the Icahn School of Medicine at Mount Sinai found that 44% of African Americans reported depressive symptoms two weeks after delivery, compared to 31% percent of white women. Are they rising? Yes, but why? NY Times says: “Postpartum depression and the larger group of maternal mental health conditions called perinatal mood and anxiety disorders are caused by neurobiological factors and environmental stressors. Pregnancy and the postpartum period are already vulnerable times for women due in part to the hormonal fluctuations accompanying pregnancy and delivery, as well as the sleep deprivation of the early postpartum period. Now, fears about the health of an unborn child or an infant and the consequences of preventive measures, like social distancing, have added more stress.” Isolation is a huge factor in mental health struggles. Isolation during the pandemic may be a factor increasing PMADs, along with the new fears that the pandemic has instilled in families. I think that social media plays a role in this as well. So many new parents have unrealistic expectations because of what they see other people share, but other people only share the good (usually). The let down parents are experiencing results in unhealthy feelings of blame and guilt or shame that they are not the best parent. In reality, we could be using social media to spread more awareness and create a better understanding of what so many people go through in pregnancy and postpartum. Another way to decrease PMADs effects on a family is to increase postpartum appointments and include a PMAD screening at prenatal and postpartum visits. Prevention is so important and a key part of preventing PMADs is increasing support. Parents should try to put support plans in place before the baby arrives. This could include a meal train, family members visiting, a babysitter, etc. Resources:
References:
Anonymous. (2018, March 16). My postpartum exercise addiction - seleni - maternal mental health institute. Seleni. Retrieved May 11, 2022, from https://www.seleni.org/advice-support/2018/3/16/my-postpartum-exercise-addiction Heyman E, Gamelin FX, Goekint M, Piscitelli F, Roelands B, Leclair E, Di Marzo V, Meeusen R. Intense exercise increases circulating endocannabinoid and BDNF levels in humans--possible implications for reward and depression. Psychoneuroendocrinology. 2012 Jun;37(6):844-51. doi: 10.1016/j.psyneuen.2011.09.017. Epub 2011 Oct 24. PMID: 22029953. Kozhimannil, K. B., Trinacty, C. M., Busch, A. B., Huskamp, H. A., & Adams, A. S. (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric services (Washington, D.C.), 62(6), 619–625. https://doi.org/10.1176/ps.62.6.pss6206_0619 Lakshmin, P. (2020, May 27). Experts fear increase in postpartum mood and anxiety disorders. The New York Times. Retrieved May 6, 2022, from https://www.nytimes.com/2020/05/27/parenting/coronavirus-postpartum-depression-anxiety.html Ruehle, S., Rey, A. A., Remmers, F., & Lutz, B. (2012). The endocannabinoid system in anxiety, fear memory and habituation. Journal of psychopharmacology (Oxford, England), 26(1), 23–39. https://doi.org/10.1177/0269881111408958 Birth psychology, also called “prenatal and perinatal psychology” or “reproductive psychology” is the field of study dedicated to psychology in utero and how the mental state of a parent impacts the baby, not just throughout pregnancy, but over the course of their life. This field also covers the psychology of reproductive health, fertility, pregnancy and infant loss, and how birth control impacts psychology. Birth psychology is just beginning to gain more attention as we see the long term effects of stress in pregnancy and the way sleep training can impact mental health long term, but I believe this field should be getting even more attention, especially with the rise of PMADs. As we begin paying more attention to PMADs and how they impact family dynamics, we also begin to see how they impact infants. PMADs is the acronym for Perinatal Mood and Anxiety Disorders. These negatively impact babies and the bonding between parent and baby. I think an important part of healing PMADs is healing the bond between family members affected. This is not the main focus when a mental health crisis occurs, but when we are at a point in care where we can begin focusing on healing our relationships with others (after we heal our relationships with ourselves) this is an important step. “When untreated in a primary caregiver, PMADs adversely affect parental cognitions and beliefs, attachment to the infant, and the growing caregiver-infant relationship. PMADs affect early developmental outcomes of infants including neurosynaptic development, regulatory development, and developmental milestones.” (Hoffman 2016) The Children’s Hospital of Philadelphia says: “When a PMAD goes untreated, it can have unwanted and negative effects on your family. Research shows that depressed and anxious parents often smile less, talk less, and are less likely to touch or engage with their newborns throughout the first year of life.” Not only those in mental health should be aware of why birth psychology education could help in the care they provide families, all people working with expectant families and families of infants should have a basic education around birth psychology. Neonatologists should be aware that children of mothers with PMADs have increased risk of prematurity, sudden infant death, and need for neurodevelopmental and neurobehavioral support services. Child behavioral specialists may even find a link between a certain behavior a child is expressing and an insecure attachment/bond with their parent linking all the way back to pregnancy. Children of parents with depression and anxiety often develop learning, attention or behavioral difficulties as they grow older. Older children may suffer from the loss of maternal/paternal attention and support by becoming depressed or anxious as teenagers. Pregnancy is the root of where our development begins and oftentimes the root of where healing is needed. That is why it is important for both practitioners and parents to have an understanding. Including this topic in curriculum, as a CEU for providers, and in newborn care and childbirth education courses are just a few ways we can begin making this information more widely known, but here are a few tips for expectant parents and parents of infants wanting to heal an insecure attachment or promote a healthy bond right now. How can you promote birth psychology throughout birth, pregnancy, and postpartum? Developmental Milestones and Opportunities for Connection in Pregnancy: Tactile sensitivity begins in the seventh week of gestation and steadily enlarges to include most parts of the body by seventeen weeks and all parts by thirty-two weeks. There are many ways to see a physical reaction and know for yourself that your baby is responding! Talk to your baby! Hearing may begin early in the first trimester or as late as eighteen weeks. Speaking to your baby is a great way to begin bonding. Your baby will begin recognizing your voice specifically. This is a great way to check in with your baby about the emotions you are experiencing. Stress is a normal part of life, but telling your baby what is happening and why can reduce the impacts of stress long term. Interact with your baby! The fetus is aware of light even while the eyelids are still fused together and will react to lights flashed on the abdomen. You can try playing with a flashlight on your abdomen, moving your hands along your abdomen and following your baby as they follow the light. You can also try interacting through noise such as music. You may find your baby prefers Taylor Swift over Beethoven or vice versa! Dreaming Premature babies dream more than anybody else! They show the most smiles, frowns, finger movements, neck stretches, mouth movements, and vocalizations in their dreams. Ultrasound has shown that the beginning of REM/dreaming activity is at just twenty-three weeks! Remember... Your baby is connected with you and is experiencing your emotions on an even deeper level. While it can be important and effective to reduce stress and keep a positive mindset it can also be important to discuss feelings and experiences directly with your baby. This not only teaches emotional regulation, but also offers more bonding opportunities. Try following Karen Strange’s communication tips: 1. Tell your baby what you are going to do BEFORE you do it 2. Tell your baby what is going on 3. Tell your baby what you want them to do 4. Tell your baby the story of what happened When it comes down to it, all your baby wants is to feel how we all want to feel; wanted, welcome, seen, heard, felt, safe, protected, a sense of belonging, and loveable! Four Goals for your Bonded Birth:
Speak to your baby and hold healthy eye contact! Your baby communicates through the universal language of emotion. Our eyes hold much emotion. They are a way we recognize each other and a way that we show we are listening fully. When speaking with your baby, practice holding eye contact. You can look them in the eyes and blink until they begin blinking in sync with you, a bonding exercise! Skin to skin, anytime! Skin to skin is not just important during immediate postpartum. It should be done well into the weeks following, between both parents. It is a great way too bond and should even be done during bottle feeds. During bottle feeds remember to alternate which side you are feeding on, the same way you would with the breast. Family Focused Stress Relief Sometimes whole family focused stress relief is extremely necessary when a parent is home all day and the other is not. The working parent may come home happy, but actually be bringing in more stress because they are not practicing family focused stress relief. The root prevention for this is setting up support systems. Non Gestational Parents: Oftentimes non gestational parents struggle to bond the same way the birthing parent does. This can happen in couples where neither parent is birthing the baby (adoption, surrogacy, etc). These feelings are normal and valid. I think it is important to remember here that so many bonding techniques for straight couples conceiving and birthing a baby do work for LGBTQIA+ community members and non gestational parents of any kind, as well.
Another huge bonding tool, one on one time. One of the biggest recommendations I have for new parents is for the working parent to set up one on one time with the baby. This allows bonding and allows them to care for their partner. Their partner can get to bed early or take some alone time while the working partner is caring for the baby. This could be an hour in the evening just to help with the bedtime routine. Snuggles, stories, and the final feeding done by the working parent while the birthing parent rests or takes a sitz bath. Maybe afterwards you eat dinner together if your baby is asleep and the gestational parent is awake Find a routine that works for your family and allows bonding between all parties. Becoming parents is one of the two top ways to heal insecure attachment. You are a safe haven and secure base for your baby AND for your partner. By caring for ourselves we care for others indirectly, what will that look like for your family? References:
Hoffman C, Dunn DM, Njoroge WFM. Impact of Postpartum Mental Illness Upon Infant Development. Curr Psychiatry Rep. 2017 Nov 6;19(12):100. doi: 10.1007/s11920-017-0857-8. PMID: 29105008. Johnson Rolfes, J., Paulsen, M. Protecting the infant-parent relationship: special emphasis on perinatal mood and anxiety disorder screening and treatment in neonatal intensive care unit parents. J Perinatol (2021). https://doi.org/10.1038/s41372-021-01256-7 White, K., & Martin, M. (2012). Pre-and perinatal experiences for health and healing. Pathways to Family Wellness, winter (36). Wirth, Frederick. (2001). Prenatal Parenting. HarperCollins. Surgery Induced Menopause2/4/2023 Menopause represents the permanent cessation of menstrual periods and the loss of fertility due to the loss of ovarian function. It can occur spontaneously (natural menopause) or it can be surgically induced by bilateral oophorectomy. A bilateral oophorectomy is the removal of both ovaries. Menopause usually takes place in women between the ages of 45 and 55. A women is officially in menopause when her periods have stopped for 12 months. Some will begin to experience perimenopausal symptoms years before that time. Symptoms are caused by estrogen levels decreasing. In natural menopause they decrease slowly over time, but what happens when they suddenly drop after surgery? What is surgery induced menopause? Surgical menopause occurs when premenopausal women have their ovaries surgically removed in a procedure called a bilateral oophorectomy. This causes an abrupt menopause, with women often experiencing more severe menopausal symptoms than they would if they were to experience menopause naturally. Surgery induced menopause is most common after a radical hysterectomy that removes the ovaries. Each year about 600,000 women in the United States undergo a hysterectomy. 55% and 80% of these women also have their ovaries removed along with the uterus. What are the risks?
Common Surgeries Leading to Surgery Induced Menopause: In most cases, removing the ovaries is a preventive measure against disease. In some cases it’s performed alongside a hysterectomy, a procedure that removes the uterus. Prophylactic ovary removal: Prophylactic ovary removal is usually performed by a gynecologist. There have been some cases in which early ovarian cancer has been found during prophylactic ovary removal. This has led many high-risk women to choose to have their ovary removal done by a gynecologic oncologist. A series of tests are run before prophylactic ovarian removal including:
Laparoscopic ovary removal: Laparoscopic ovary removal is usually performed in the hospital or outpatient surgical center under general anesthesia. In some cases, the surgery can be done using local anesthesia. Abdominal ovary removal: Abdominal ovary removal is performed under general anesthesia and generally lasts about 1-2 hours. It may last longer if the surgeon needs to do some further exploration. Salpingo-oophorectomy is the removal of the fallopian tube (salpingectomy) and ovary (oophorectomy). Elective salpingo-oophorectomy represents the removal of ovaries and fallopian tubes in a woman without indication for this procedure. Risk-reducing salpingo-oophorectomy is defined as the removal of ovaries and fallopian tubes in a woman with hereditary ovarian cancer syndrome. Indications for salpingo-oophorectomy in low-risk patients:
Indications for salpingo-oophorectomy in high-risk patients:
Advantages of Bilateral Salpingo-Oophorectomy (SO):
Support Doctors may recommend hormone replacement therapy. HRT counteracts the hormones you’ve lost after surgery. HRT also lowers the risk of developing heart disease and prevents bone density loss and osteoporosis. This is especially important for younger women who have removed their ovaries before natural menopause. Current international guidelines (6) advise use of MHT for all women who undergo menopause under the age of 45 years provided that they do not have other contraindications to MHT (6). Treatment should continue until the average age of menopause (51 years) and then be reviewed. Use of MHT will resolve hot flushes and sweats in 80-90% of women, although there is evidence that hot flushes and night sweats as well as vaginal dryness may persist despite MHT use in younger women. There are no specific guidelines on the type of MHT to use but oestrogen only MHT is generally prescribed for those women who have had a hysterectomy (removal of the uterus). Women who retain their uterus should use an oestrogen and progestogen combination preparation. Support from friends, family, and especially your partner is extremely important and can ease the transition. For Hot Flashes:
For Stress:
New Research A new study is actually suggesting that surgery induced menopause is no worse than natural when it comes to anxiety and depression. In the Study of Women’s Health Across the Nation (SWAN), Dr. Hadine Joffe from the CWMH assessed depression and anxiety symptoms annually for a period of up to 10 years. During the 10 years of follow-up, 1,793 (90.9%) women reached a natural menopause, 76 (3.9%) reported a hysterectomy with ovarian conservation, and 101 (5.2%) reported a hysterectomy with bilateral oophorectomy. For all groups of women, depression scores decreased from the time of the last menstrual period to the end of the study at about the same rate.Those who experienced surgically induced menopause did not report higher rates of negative feelings than those with natural menopause. While physical symptoms are more intense this study suggests that mentally natural and surgical menopause are the same. Surgery induced menopause s caused by big shifts in hormone levels in the body, specifically estrogen levels. Those considering surgery that has menopause as a side effect will want to discuss what to expect with their provider and inquire about hormone replacement therapy. This is another situation where it is great to put plans for support in place beforehand. It can also be helpful to keep your partner informed so they can better support you! References:
Finch A, Metcalfe KA, Chiang JK, Elit L, McLaughlin J, Springate C, Demsky R, Murphy J, Rosen B, Narod SA. The impact of prophylactic salpingo-oophorectomy on menopausal symptoms and sexual function in women who carry a BRCA mutation. Gynecol Oncol. 2011;121(1):163-8. Hickey M, Davis SR, Sturdee DW. Treatment of menopausal symptoms: what shall we do now? Lancet. 2005;366(9483):409-21. Secoșan, C., Balint, O., Pirtea, L., Grigoraș, D., Bălulescu, L., & Ilina, R. (2019). Surgically Induced Menopause-A Practical Review of Literature. Medicina (Kaunas, Lithuania), 55(8), 482. https://doi.org/10.3390/medicina55080482 Trying to conceive can be a stressful process, even when the goal is to keep it fun. It is important to consult with your provider to discuss ways to increase your chance of success, but remember; many ways can increase odds of conception that may not be your provider's typical recommendation. Some of these less conventional recommendations may even be important to continue throughout pregnancy. Here are our top 10! 1. Have sex every day! Research shows that couples with the highest rate of pregnancy have sex as often as possible. Especially as often as possible close to ovulation! Sperm can live in the body for up to 5 days so don’t stress if you do end up missing a day. It is important to get into this pattern before trying to conceive so that it does not feel like added stress. It should be something you enjoy doing and are already used to doing before you add on the other stresses trying to conceive can bring. Remember, even if you use a fertility tracking app it may not be accurate. There is limited research proving accuracy in these methods of tracking ovulation. It can be better to play it safe and have sex more often when trying to conceive! 2. Don't rush to clean up after! Try laying for 10-15 minutes or even taking a cat nap after sex. Rushing to clean up risks the loss of sperm by not even giving them the chance to travel. Standing up can shift and move the position of sperm. Treat sex as an extremely relaxing experience and get a bit of rest after. Maybe even try a peaceful meditation to keep your stress levels low and let your body do its thing! 3. Have Fun! Sex should not feel like a business. Your stress levels rise when you treat it as work rather than play! Increased cortisol, the stress hormone, can cause a delay in success when trying to conceive. We all know the story of the couple that decided to stop trying and then got pregnant shortly after. Try switching up your usual routine to make sex more fun. It is easy to feel trapped in a routine and treat sex as a normal daily chore when you are TTC. It is important to also not to pressure yourself to have fun and relax. Try just going for it when you’re in the mood, less thinking and more doing. 4. Keep your womb warm! Traditional Chinese Medicine practitioners recommend keeping your womb warm. Kirsty Eng, a Traditional Chinese Medicine practitioner says “Yang warming energy is the origin of movement of blood and qi throughout the body. It is also the catalyst for reproductive processes, like ovulation and implantation. Yang energy, being also uplifting and supportive in nature, is also responsible for allowing a pregnancy to continue.” A Yang deficiency refers to a cold womb. A warm womb has good blood flow. To promote a warm womb you can try eating warm foods and drinks, keeping your feet warm, avoiding sitting on cold surfaces, avoiding swimming when menstruating, and trying acupuncture! 5. Ditch the alcohol! Limiting alcohol is not just good for a developing baby! It is also good for you and your partner. Limiting alcohol can benefit a higher sperm count. Drinking can prevent ovulation, although researchers are unsure as to why. It can also prevent a fertilized egg from implanting. One study, by Human Reproduction, found that the more a woman drinks the less likely she becomes to conceive. The results from this article stated, “moderate to heavy drinking during the luteal phase, and heavy drinking in the ovulatory window could disturb the delicate sequence of hormonal events, affecting chances of a successful conception.” 6. Maintain a healthy weight! Being either over or underweight can impact your ability to conceive. For someone overweight, it may take twice as long to conceive and four times as long for someone underweight. This goes for you and your partner! While estrogen is produced at a higher rate in obese women, obesity in males can disrupt the endocrine system. This affects sperm viability and the chance of successful pregnancy. Increased estrogen can cause interference with ovulation. Being underweight can cause disruption in ovulation as well, and a loss of periods altogether (amenorrhea). Starting a workout routine can be a fun activity to do with your partner and may benefit you both. Exercise reduces stress by increasing endorphins and reducing cortisol levels (your stress hormone). Reduction of stress has been proven to increase the chances of conception. Exercise also helps you sleep better and a good circadian rhythm also increases those chances of conception! Continuing to exercise during pregnancy reduces the risk of some health issues in pregnancy. 7. Quickies Count! Remember, documentaries are great, but short films are entertaining too! There is no research connecting the length of sex and chance of getting pregnant so as far as we know, they count too! Your chances are just as high with a quickie and they can be fun! They also come in handy when you’re tracking ovulation and may have limited time to have sex, but need to do so immediately. We do recommend that you still aim to orgasm, for pleasure purposes because some professionals believe this can increase the chance of success when TTC. 8. Improve your wellness! Research has proven that what you put on your skin and what you put into your body affects the chances of conception. Improve your diet by eating antioxidant-rich foods, leafy greens that are high in folate, more fiber, and fewer carbs. Try including quinoa, beans, lentils, avocados, Greek yogurt, cheeses, salmon, and sunflower seeds in your diet. Many beauty products are unsafe to use when pregnant and maybe even when trying to conceive. Always read the label when purchasing products or speak to your doctor. Try to avoid salicylic acid, retinoids, chemical sunscreens, benzoyl peroxide, and hydroxy acids. 9. Start a project! The countdown of DPO (days past ovulation) can feel like an eternity. It is important to reduce stress during this period as well. The best way to do that? Find something else to focus on. Make a list of projects you have been meaning to start or hobbies you have wanted to attempt picking up. Maybe a good project would be researching meal planning or starting a relaxing workout routine. Just keep yourself focused on other things in addition to TTC. You don’t want to lose sight of who you are and what you enjoy or add additional stress to your life. 10. Tone your uterus Exercise is not the only method you should use to tone your uterus. Herbal teas can be used to tone the muscles of your uterus too! Red raspberry leaves are commonly used to tone the uterus, but we also recommend using saffron, lemon balm, and Dong Quai. Dong Quai increases the circulation of blood to the uterus and is iron-rich. It tones the uterus by regulating hormonal control and menstrual cycle rhythm. This can also help those with endometriosis, uterine cysts or fibroids, ovarian cysts, can improve your immune system, and can decrease cramping. Lemon Balm supports healthy stress responses and can decrease anxiety and depression. With TTC being a stressful experience for many, but one that requires low stress to be successful, lemon balm is important. Saffron can increase your sex drive! This is great during a time when you are trying to have sex as often as possible, but have as much fun as possible. This works for both men and women by increasing blood flow in the pelvic region. References:
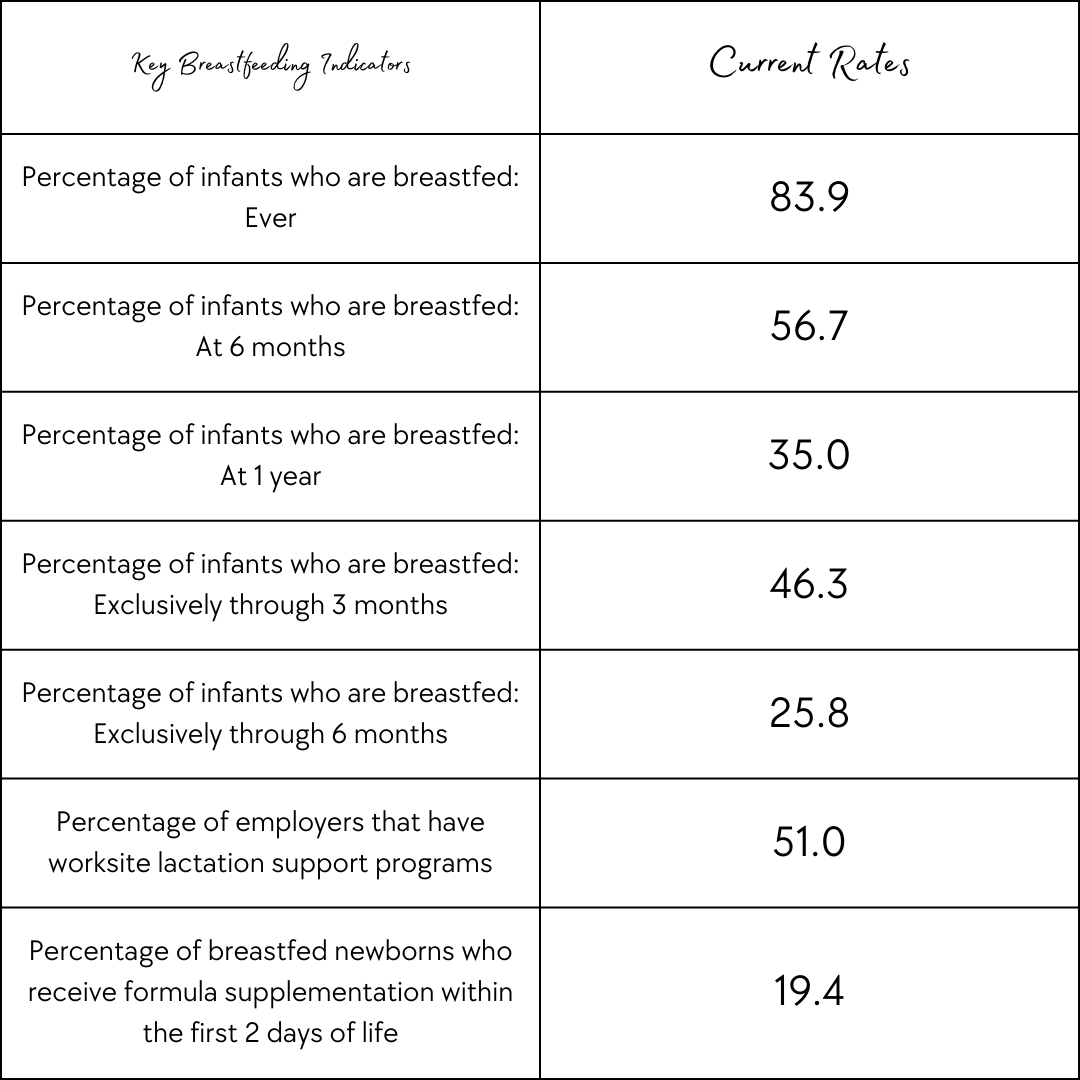
Barton, D. (2021, May 7). How to use fertility herbs to enhance your fertility naturally. Natural Fertility Info.com. Retrieved February 12, 2022, from https://natural-fertility-info.com/fertility-herbs Eng, K. (2018, October 30). You need a warm womb! Kirsty Eng. Retrieved February 12, 2022, from https://kirstyeng.com.au/blog/you-need-a-warm-womb/ Laurel (2021, October 5). 10 foods to eat to increase fertility. Laurel Fertility Care. Retrieved February 12, 2022, from https://www.laurelfertility.com/foods-to-eat-increase-fertility/ Mayo Clinic Staff. (2020, August 18). Exercise and stress: Get moving to manage stress. Mayo Clinic. Retrieved February 12, 2022, from https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/exercise-and-stress/art-20044469 Mohammad Yaser Anwar, Michele Marcus, Kira C Taylor, The association between alcohol intake and fecundability during menstrual cycle phases, Human Reproduction, Volume 36, Issue 9, September 2021, Pages 2538–2548, https://doi.org/10.1093/humrep/deab121 Stroud, K. (2020, August 29). How to care for your skin when trying to conceive, pregnant or nursing. Dermstore. Retrieved February 12, 2022, from https://www.dermstore.com/blog/skin-care-ingredients-avoid-pregnant/ (n.d.). How Fast Can You Get Pregnant? - New Kids Center. Retrieved February 12, 2022, from https://www.newkidscenter.org/How-Fast-Can-You-Get-Pregnant.html Zwingerman R, Chaikof M, Jones C. A Critical Appraisal of Fertility and Menstrual Tracking Apps for the iPhone. J Obstet Gynaecol Can. 2020 May;42(5):583-590. doi: 10.1016/j.jogc.2019.09.023. Epub 2019 Dec 25. PMID: 31882289. What started as a scientific campaign to promote the research showing that breastmilk is the best option for infants has now turned into an intense pressure that leaves parents who cannot or choose not to breastfeed feeling ashamed and inadequate. “Breast is Best” is the notion held by many organizations parents and providers respect, like the World Health Organization. The goal was to inform expectant parents of the benefits of exclusive breastfeeding. Exclusive breastfeeding is breastfeeding as the only form of feeding for at least the first six months of life. This campaign started in the 1960s or 70s, although the exact origin is still unknown. The campaign has normalized breastfeeding in public and increased rates of families attempting to breastfeed. People feel empowered to pump at work and advocate for their rights around lactation and the workplace. Some of the benefits of breastfeeding include that the nutrients of breastmilk are better absorbed by your baby and are the best to support brain and nervous system development. Certain fats in breast milk help with eyesight. Breastfeeding lowers the risk of SIDS (sudden infant death syndrome) and helps strengthen a baby’s immune system, but how many people stick with breastfeeding when they leave the hospital? How many people actually exclusively breastfeed? There are many things that impact the rate of parents breastfeeding. Some parents simply do not have the option because they do not lactate. Others want to, but struggle because of barriers making it hard to access lactation support or make breastfeeding a sustainable option long term. We have come a far way with workplace breastfeeding and pumping rights, but we still have a long way to go. What are the barriers to breastfeeding? One of the biggest reasons parents choose not to breastfeed is because of a barrier in place. In most cases, a decision not to breastfeed has a reason behind it. Barriers can include lack of knowledge, societal norms, lack of support, employment and child care, barriers to health services, and various lactation problems. While the “Breast is Best” campaign did increase education it did not remove all of these barriers. Even without all of these barriers it comes down to something really simple, it is the parents' choice if they want to breastfeed, bottle-feed pumped milk, or use formula. The first recommendation from the American College of Obstetricians and Gynecologists (ACOG) is that “Parents have the right to make their own informed choice about whether or not to breastfeed”. Providers are meant to provide unbiased non-coerced support. Despite this recommendation, many parents still feel like they do not have a choice. When they cannot breastfeed they feel like they are letting their baby down. Breastfeeding May Better Your Mental Health, But The Pressure to Breastfeed Does Not Breastfeeding supports hormonal processes that induce the release of oxytocin. Oxytocin helps with parent-infant bonding and lowers cortisol levels. Cortisol is the stress hormone and higher rates lead to mental health problems. Breastfeeding parents are more likely to report positive mood, less anxiety, and increased calm according to Frontiers in Global Women’s Health, but it is not reported how many months into breastfeeding the parents in this report were. The pressure to breastfeed begins far before the baby arrives. The decision to breastfeed is typically made before or during pregnancy. It is something a lot of parents think about when trying to conceive. Parents research the best pump, best chair to nurse in, and most comfortable nursing bras. By just three months less than half of the babies in the U.S. are breastfed exclusively. This drops to 25% by six months. Despite this, there is still intense pressure to breastfeed that takes a huge toll on parents' mental health. The pressure comes from health care providers, some of which do not even choose to breastfeed their children. It comes from lactation consultants and even from other moms who think they know best for every mom. The truth is, they don’t. Only you can decide if breastfeeding works for your family and that decision may change over time. When beginning your breastfeeding journey it may start rocky and improve or it may start great and take a toll on you later. It may be a combination of things taking a toll whether that is lack of sleep catching up to you or something else. Only you know your body and your mind, and you know when you have reached your limit. All of those voices telling you what they believe you should do for your baby can take a toll. From Facebook groups to online forums to moms at playgroups, people love to try to tell other parents how to parent. The psychological pressure to breastfeed can increase the risk of postpartum depression. The feeling that you are unable to reach the goal you set for yourself can feel very defeating. That feeling may contribute to postpartum depression and other postpartum mood and anxiety disorder symptoms. Nursing For Women's Health released a piece supporting the idea that more research is needed on what the pressure to breastfeed is doing to the mental health of parents. The signs of mental health decline could include feelings of sadness, anxiety, fear, trouble sleeping, anger, or irritability. More information on postpartum mood and anxiety disorders (PMADS) can be found here. While this research may currently be limited, many parents are still speaking out about the way this pressure has affected them personally. Recent trends in childbirth can even impact the success of breastfeeding despite so many hospitals being part of the “baby-friendly hospital initiative”. This initiative supports early initiation of breastfeeding, skin to skin, delayed cord clamping, and more parent-baby bonding techniques, but providers following this method have been reported of holding formula hostage when families request it and ignoring the recommendation by the ACOG that parents have a unique perspective and know what is right for their baby. What if I can’t breastfeed? We live in a world with a lot of options and those options are becoming more and more accessible as this discussion on the reality of breastfeeding becomes more discussed. If providing your baby with breastmilk is important to you you may be able to pump or try donor milk. You may decide the formula in combination with breastmilk works best for your family or you may choose to exclusively feed your baby formula. There are many options when it comes to formula because just like breastfeeding there is no one option that works for everyone. When exploring formula options you can find a variety of brands and a variety of recipes within each brand. Some formula recipes are designed to support a sensitive stomach or designed for premature babies. If you are choosing formula; just like deciding what feeding option you will use, you will decide which formula type is best for your baby. At the end of the day, the most important thing is that your baby is fed and that you are not pouring from an empty cup. A fed baby is a healthy baby. “Fed is Best” is a movement to help normalize all feeding options. The goal is to remind parents that what is healthy is that their baby is fed. The organization offers various resources to avoid harm to the physical health of infants who need the formula and the mental health of parents being pressured to breastfeed. Remember, to avoid pouring from an empty cup you need to care for yourself. Breastmilk may be ideal for each infant, but it is not always ideal for each parent. The “Breast is Best'' movement should not only increase education but also strive to break down barriers to breastfeeding for those who wish to breastfeed. As a society, we should strive to create an inclusive community for parents that offers empathy and understanding when a parent decides to do something healthy for their family but is not a choice we would have made ourselves. Each family is different, but so is each baby. What worked with one may not work for your next. References:
C. D. C. (2021, November 24). Breastfeeding report card. Centers for Disease Control and Prevention. Retrieved February 13, 2022, from https://www.cdc.gov/breastfeeding/data/reportcard.htm C. D. C. (2021, August 24). Facts. Centers for Disease Control and Prevention. Retrieved February 13, 2022, from https://www.cdc.gov/breastfeeding/data/facts.html J, H. (n.d.). Breast milk is best. Johns Hopkins Medicine. Retrieved February 13, 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/breastfeeding-your-baby/breast-milk-is-the-best-milk Office of the Surgeon General (US). (1970, January 1). Barriers to breastfeeding in the United States. The Surgeon General's Call to Action to Support Breastfeeding. Retrieved February 13, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK52688 The light isn't green forever. AuthorJess Kimball is a Full Spectrum Doula and Certified Lactation Counselor trained in Ayurvedic and Chinese medicine. |
|
EST. 2016
North Carolina | Vermont Jess Kimball |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
Jess Kimball provides doula care, birth photography, and a variety of other services to families!
|
 RSS Feed
RSS Feed